Getting to know sarcoma with Dr. Philip Friedlander
2020-07-01
In honor of sarcoma awareness month, UCIR spoke with Dr. Philip Friedlander – an oncologist at Mount Sinai in New York. Dr. Friedlander is currently an investigator on a clinical trial that involves immunotherapy treatment for patients who have Kaposi sarcomas.
What is sarcoma?
Dr. Friedlander: Sarcoma is a type of cancer that starts in what are called “mesenchymal cells.” There are many different types of sarcomas, with about 80% starting in soft tissue, like muscle or skin, and most of the remainder starting in bone.
Who is sarcoma most likely to affect?
Dr. Friedlander: Sarcomas are a rare type of cancer, representing approximately 1% of all adult cancers. Unfortunately, sarcoma is a cancer that often occurs in children. It can occur in almost any body part, presenting as a growing mass. Certain types of sarcoma, such as Kaposi sarcomas, occur more frequently in people who are immunocompromised, like people with AIDS for example. These types of sarcoma are usually associated with a type of virus called herpes virus 8, and patients who are immunocompromised are predisposed to this virus.
What are the signs and symptoms of sarcoma to look out for?
Dr. Friedlander: Patients with sarcoma may notice a mass that is growing, or they may notice symptoms associated with a mass, like pain or discomfort. Patients who develop Kaposi sarcomas could have purple-ish lesions growing on their skin.
How is sarcoma usually treated and how effective is treatment?
Dr. Friedlander: Sarcomas are a very broad group of cancers and there is a lot of variety between them, so they may be treated in different ways. In many cases they are treated surgically, but depending on the type of sarcoma, radiation or chemotherapy might be used – with mixed success. Some types of sarcomas, such as gastrointestinal stromal (GIST) tumors, have specific mutations, which make them particularly sensitive to targeted chemotherapies that can shrink the tumors or prevent progression of the cancer, but these benefits are often only temporary. When sarcomas have spread to many different locations, we don’t have a proven cure for it.
What immunotherapies have been tested or approved for the treatment of sarcoma?
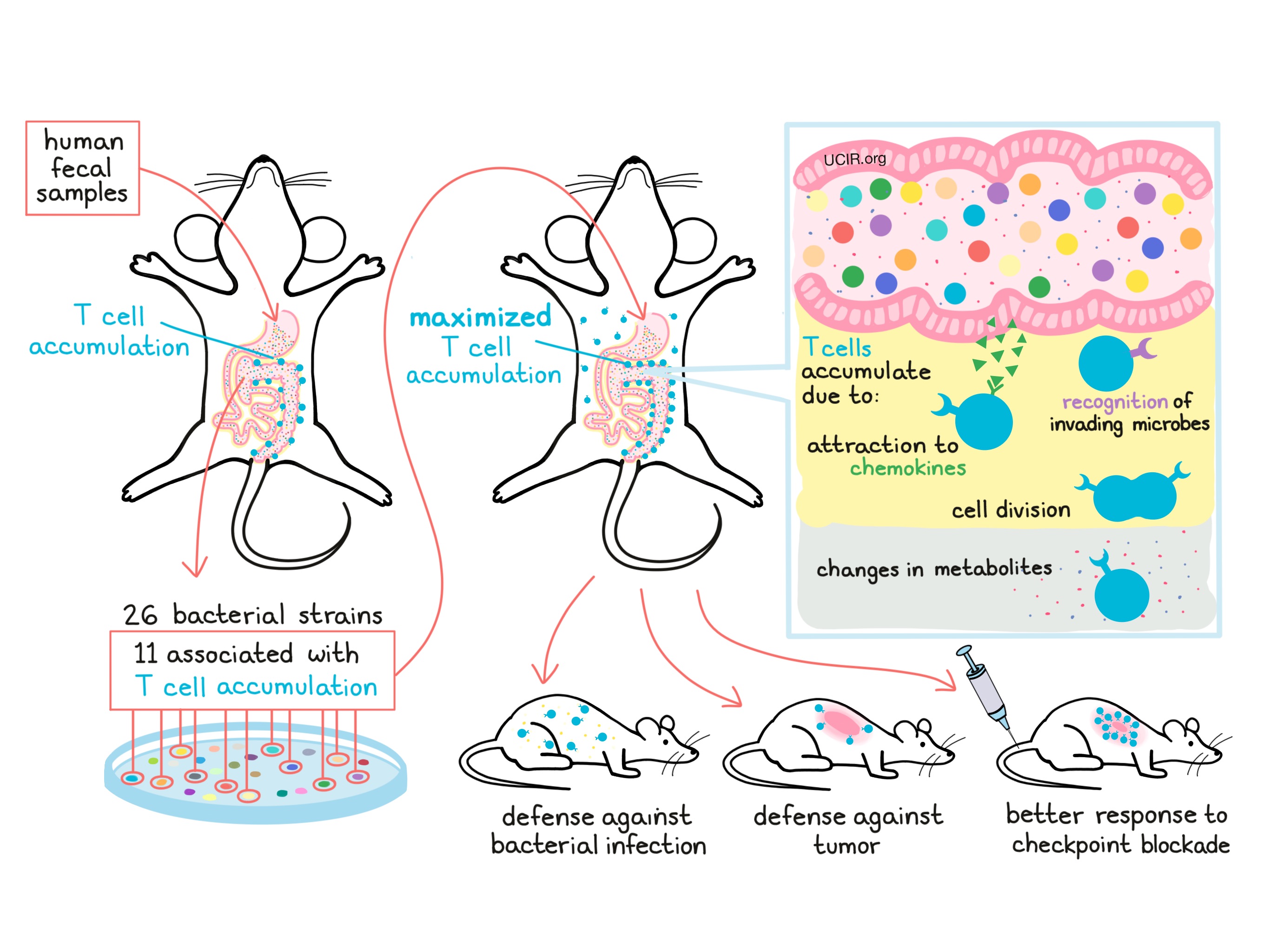
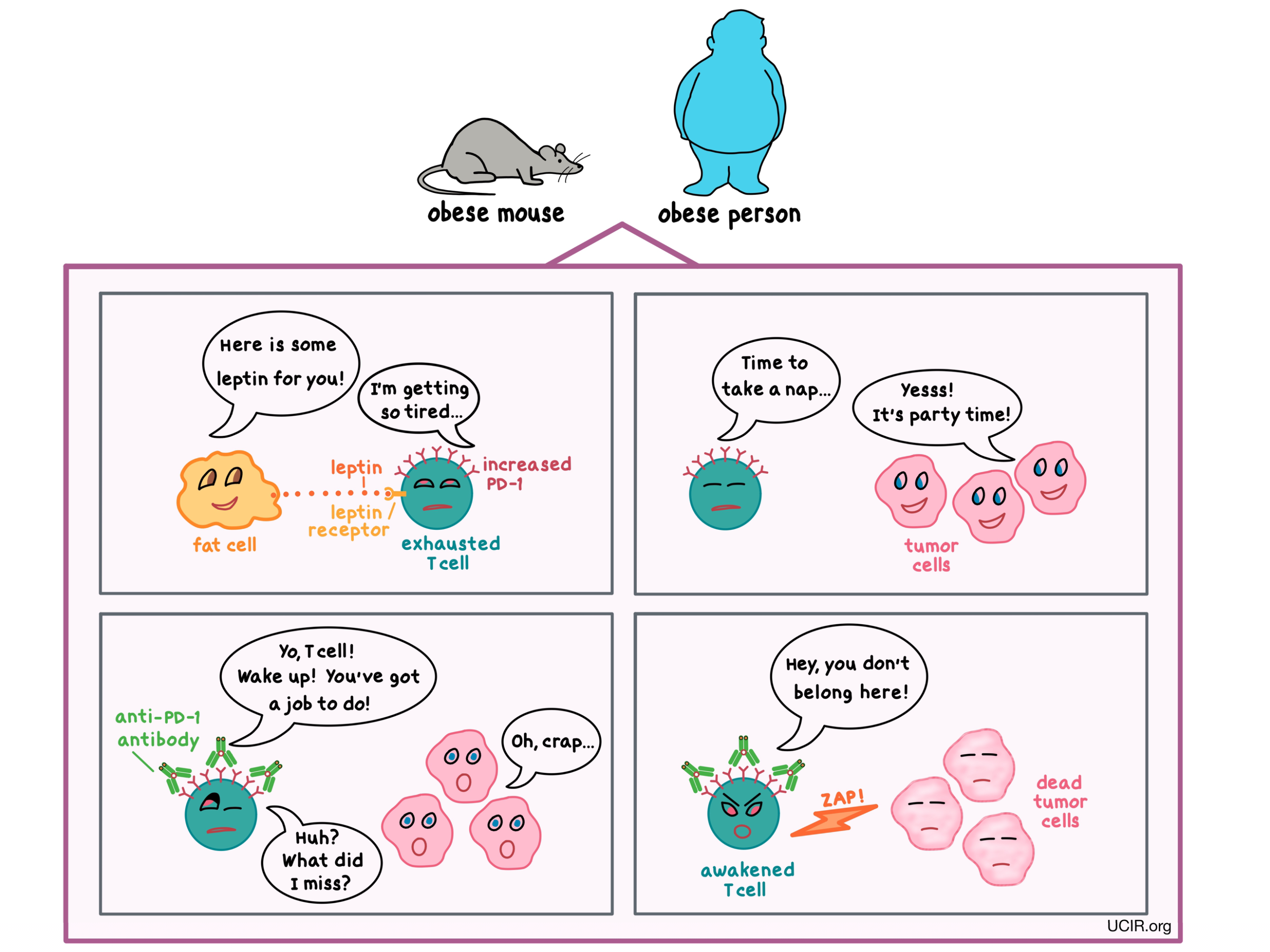
Dr. Friedlander: So far there are a number of immunotherapy options for sarcoma that are undergoing testing. Research in sarcoma is more challenging than in some other cancer types because you have a broad range of subtypes and they don’t all respond the same, so you really have to look at the various subtypes individually. For example, there has been a lot of testing of a type of immunotherapy known as checkpoint blockade – antibodies that block certain components of the immune system, allowing it to be more active. Specifically, inhibitors of PD-1 and PD-L1 keep T cells active in the area of the cancer so they can be more effective in killing cancer cells. In sarcoma, this strategy has been looked at and in some cases there has been early evidence of responses, but only in certain subsets of patients. Larger studies are now being done. There has also been work combining inhibitors of PD-1 or PD-L1 with inhibitors of CTLA-4 – another checkpoint that works differently than PD-1 – or with an oral medication called axitinib that blocks blood vessel formation. In some cases, combination treatments like these improved responses.
Another thing we look at in oncology is something called microsatellite instability, which is related to certain types of changes in the DNA of the cancer cell. If a patient has a high degree of microsatellite instability in their cancer, then there is actually an FDA-approved PD-1 inhibitor that can be used regardless of the cancer type. This can happen sometimes in advanced soft tissue sarcomas.

What is happening in the clinical trial you are working on?
Dr. Friedlander: Here at Mount Sinai, we’re a part of a national study looking at the PD-1 inhibitor pembrolizumab in patients with HIV who have developed Kaposi sarcoma. The trial we’re working on is looking broadly at patients with Kaposi sarcoma who have either disseminated disease (meaning it has spread to different parts of the body) or relapsed/refractory disease (meaning the cancer went away but came back after prior treatment, or did not respond to prior treatment). Patients with HIV have an increased risk for this type of cancer due to its association with a virus called the Herpes 8 virus, or HHV8. This approach is considered investigational for this cancer, and all the more so in patients with HIV, whose immune systems are already altered. Because immunotherapies further affect the immune system, you have to be very careful in terms of what interactions there will be, because there are risks for immune-related toxicities and inflammation in various parts of the body. We also have a broader trial that’s looking at the best ways of administering checkpoint blockades and the best ways of combining them with other treatments. It’s a phase 1 study, so that means we are mostly investigating safety and toxicity, but we are also looking out for signals of efficacy.
How promising is cancer immunotherapy as an approach to treat sarcomas?
Dr. Friedlander: Well, the immune system is very complicated, so I think to answer that, we need to learn more about what is not working well in the immune system of patients with specific types of sarcomas and then figure how best to leverage that information to find ways to improve it. While I have mentioned just a few, there are many other regulators of the immune system – both positive and negative. We don’t yet know about all of the specific abnormalities in each type of sarcoma, so that needs to be looked at very systematically. I think for a cancer such as a sarcoma to develop, it has to have found a way to avoid the immune system, which would usually try to kill it, because it shouldn’t be there. What we don’t know yet, and what we need to figure out, is how best to create an immunotherapy cocktail that’s somewhat personalized depending on exactly how a specific person’s sarcoma managed to avoid the immune system.
By Lauren Hitchings
References:
Dr. Philip Friedlander is an oncologist at Mount Sinai in New York, NY.