Health Inequities and Disparities in the COVID-19 Pandemic
2021-04-09
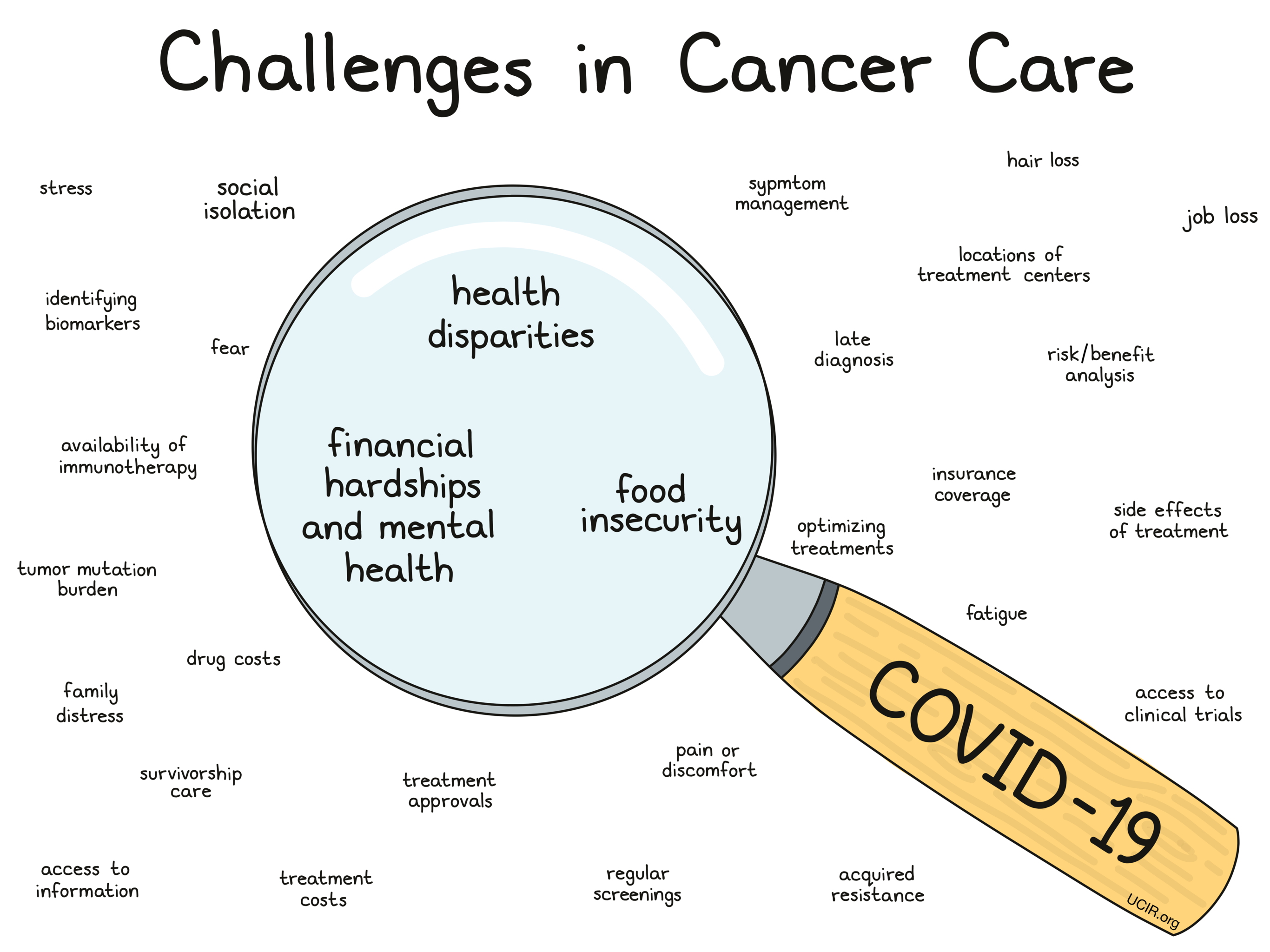
Confronting cancer is always difficult, particularly for populations underserved by the healthcare system, but confronting it in the midst of the COVID-19 pandemic raises even greater problems. Participants in a symposium at the AACR-sponsored meeting: COVID-19 and Cancer (February 3 - 5, 2021) explored causes and consequences of three major problem areas – health disparities, financial hardship and mental health, and food insecurity – all of which are exacerbated by the COVID-19 pandemic.
Health Disparities
Key takeaways
-
COVID-19 infections and deaths are proportionally greater in the black population.
-
Social and economic inequities, food insecurity, and poorer insurance coverage are a significant contributor to this disparity.
-
Outreach through community programs is essential to connect, raise trust, and educate the black community in order to improve outcomes.
Recent evidence has revealed disparities in death rates and economic impacts of the COVID-19 pandemic on different populations. For example, as of April 2020, the percentage of total deaths from COVID-19 among blacks (19%) was greater than their percentage of the population (13%). In contrast, the percentage of deaths among whites (57%) was similar to their percentage of the population (60%). Similarly, blacks suffered greater job loss or pay cuts than whites.
Many social factors contribute to these inequities:
- Dense living conditions, often with multi-generational families living together, promote infection.
- Poor access to transportation makes it more difficult to access healthcare.
- Limited sick leave in lower paying jobs makes workers in those positions more vulnerable to complications from disease and less able to recover well.
- The role of many lower paid workers in “essential” jobs that cannot be done remotely leads to greater exposure to the virus.
Exacerbating these issues, lack of health insurance, “under-insurance,” chronic conditions such as higher levels of asthma, cardiovascular disease, and cancer found in these populations increase the chances of more severe illness. Further disparities are caused by health issues associated with food insecurity. In addition, functional illiteracy, which makes it difficult to read about and manage complex therapies, as well as an absence of diversity among healthcare workers (e.g., only 3% of oncologists are black) leads to misinformation and distrust.
A useful way to address these issues is through community outreach programs to educate, connect, and raise trust in different communities. Mistrust can come from varied educational backgrounds between different communities, limited or poor experiences interacting with the healthcare system, and even negative historical experiences with the healthcare system that have promoted distrust.
One outrageous historical example is the “Tuskegee Study”, in which approximately 400 members of the black community who had contracted syphilis were followed by doctors, but not treated. Approximately 200 members of the community who did not have syphilis were also monitored. Over the course of the 40 year study, men died, went blind, insane, or experienced other severe health problems due to their untreated disease. The story of the study became public in 1972 and it was shut down. By then, 28 participants had died from syphilis, 100 had died from related complications, at least 40 spouses acquired the disease and passed it to 19 children at birth. For black Americans, the memory of the Tuskegee Study, and others, is a legacy that still promotes distrust and unwillingness to fully engage with the healthcare system. Latino, Native American, and other communities of color carry similar legacies. Applying resources to address these issues is critical to promoting better healthcare in these communities. Research is needed to develop and fund quality programs to bring appropriate programs to these communities. Some research and development is in progress.
Financial Hardship and Mental Health
Key takeaways
-
Patients with cancer often experience financial hardship due to the costs of care. That effect remains true in the midst of the pandemic. It is most pronounced in younger adults, those on Medicaid, and those living in rural areas.
-
The COVID-19 pandemic is likely to make the financial and insurance status of patients with cancer worse by causing delays in screening and treatment. Delay in treatment alone causes greater financial hardship as well as greater pain and suffering as patients seek care later.
-
Decreased ability of patients with cancer to work can lead to decreased access to insurance, and thus decreased access to higher quality healthcare.
-
Under- or uninsured patients with cancer are less likely to have access to advanced care such as immunotherapy and tend to have worse survival outcomes compared to patients with private insurance.
-
Delays in screening, diagnosis, or treatment due to limited or lack of insurance, or due to other factors related to the COVID-19 pandemic, can increase the number of cancer cases diagnosed at later stages, delay therapy, and delay the arrangement of palliative care. All these can increase financial hardship and suffering.
-
Among survivors of cancer, financial hardship was associated with anxiety, depression, loneliness, and hopelessness.
It is well documented that patients with cancer have significantly higher out-of-pocket healthcare costs than people with no cancer history. Average monthly costs for cancer therapy can be high: chemotherapy $1-$12,000, radiation therapy ~ $9,000, immunotherapy $10-12,000. Even with insurance, copayments can be significantly higher than the national average pre-tax income. As a result, patients with cancer report significant consequences from their expenses. 40% report trouble paying bills, 20% have difficulty paying food costs, 11% skip treatments, 12% skip doctor appointments and tests.
In addition, decreased ability to work among patients with cancer leads to decreased income and employment. These problems may also lead to loss of employer-provided insurance and decreased access to quality healthcare.
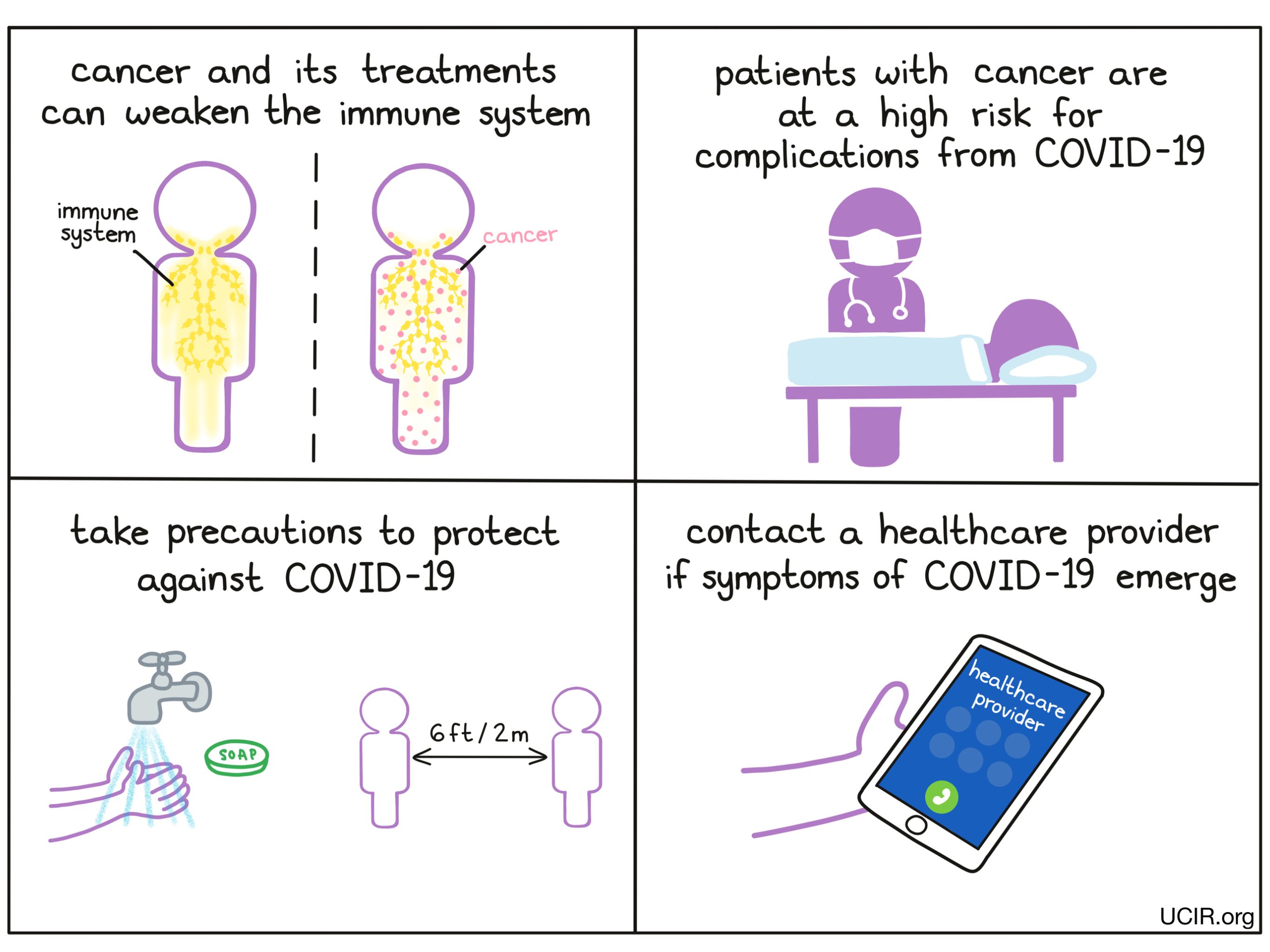
The COVID-19 pandemic is likely to exacerbate the difficult financial and insurance status of patients with cancer by causing delays in cancer screening and treatment and loss of jobs. Treatment delays alone significantly increase financial hardship. In addition, multiple studies have shown increased morbidity and mortality in patients with cancer infected with COVID-19. This is especially true for patients currently receiving chemotherapy, diagnosed with lung cancer or blood cancers, or those having completed therapy within the past 5 years. Thus, the impact of the COVID-19 pandemic on patients with cancer is likely to be severe.
To learn the effects of the pandemic on financial and mental health in survivors of cancer, researchers in one study analyzed data in the NORC COVID Impact Survey .
They asked whether the pandemic had increased financial hardship among survivors of cancer compared to other adults, what the causes of financial hardship were, and whether financial hardship led to mental health issues. The data were collected in April, May, and June of 2020. There were almost 11,000 responders to the survey, and close to 10% of these were survivors of cancer. Researchers found that:
- 1 in 5 survivors of cancer experienced financial hardship during the pandemic. This was not different for adults with no history of cancer.
- Among all the different groups of survivors of cancer, younger adults, those with Medicaid, and patients living in rural areas were more likely to report financial hardship.
- Survivors of cancer with higher education fared financially better than those without a high school diploma.
- Survivors of cancer living in suburban areas fared financially better than those living in an urban area.
- Among survivors of cancer, financial hardship was associated with anxiety, depression, loneliness, and hopelessness.
Adolescent and young adult (AYA) patients with cancer are those between the ages of 15 and 39. Due to COVID-19, these patients face additional challenges because of disrupted education, difficulty progressing in a career, and trouble achieving financial stability. In addition, they face financial challenges because of out-of-pocket costs associated with their treatment and recovery.
To explore the effects of the pandemic on this population, researchers in a second study used data collected by the Huntsman Intermountain Adolescent and Young Adult (HIAYA) Cancer Care Program, a collaborative healthcare group in Utah that provides aid to patients and survivors. The goal of the study was to explore associations between changes in employment of AYA patients and financial issues they faced during the pandemic. The data were gathered from October 2020 to the present. By the time of the AACR meeting, data from 223 patients had been analyzed.
They found that:
- Loss of jobs or hours was associated with increased financial toxicity.
- The financial well-being of women was more severely affected than that of men.
Food Insecurity
Key takeaway:
-
Food insecurity has increased with the COVID-19 pandemic and is high among both survivors of cancer and people with no history of cancer. Among survivors of cancer, food insecurity is associated with younger age, lower education, lower income, no insurance or Medicaid, and living in rural areas.
Food insecurity has increased significantly with the COVID-19 pandemic. To learn the consequences of the pandemic on food insecurity, researchers compared the prevalence of COVID-19-associated food insecurity among survivors of cancer to adults with no history of cancer. They also assessed the causes of the food insecurity. The data came from the COVID-19 household impact survey collected by the NORC COVID Impact Survey.
The population of survivors of cancer as well as that of people with no history of cancer both reported high levels of food insecurity (approximately 33%). Food insecurity among survivors of cancer was associated with younger age, lower education, lower income, no insurance or Medicaid, and living in rural areas.
Thoughts Going Forward
The presentations at the AACR session on Health Inequities highlight the many issues caused by disparities in America's healthcare system. These include loss of income and jobs, variable and often weak health insurance coverage, and delays in screening, diagnosis, and therapy due the pandemic.
All of these issues existed before the pandemic, but on a positive note, the COVID-19 pandemic has served to highlight them and make clear the breadth and depth of these problems.
In addition, by stressing the healthcare system, the pandemic has revealed additional factors that have an impact on the healthcare system. These revelations can help to identify systemic problems and, hopefully, lead to development of strategies to improve the system for all.
An important issue revealed by the effects of the COVID-19 pandemic are the many government policy decisions and subsequent plans that, although not considered healthcare issues, have major impacts on healthcare overall. For example, only 25% of a community’s health and well being is directly attributable to resources from the healthcare system. “Non-healthcare” governmental policy decisions have a greater impact. For example, infrastructure policy decisions that lead to lack of quality transportation make it difficult for many (especially people with lower incomes) to access the healthcare system. You can’t easily get quality healthcare if you don’t have a car or good transportation services to access care. Where to put the bus lines and how often they run is usually viewed as a civic policy decision – not a healthcare issue. Similarly, the availability of food resources in a neighborhood to allow for healthy food choices does not usually fall within healthcare system funding considerations. Additionally, poor housing, and the location of polluting industries can significantly affect community health, but these policies are determined by zoning laws made by civic planners, not healthcare providers. Importantly, poorer education can make it difficult to understand and manage complex medical regimens and even access and understand resources that promote healthful living – again, an issue that does not fall within healthcare discussions and planning.
Keeping these issues in mind broadens thinking about approaches to improve healthcare for a wider/more diverse group of people. The limitations in our healthcare system that the COVID-19 pandemic has made clear will hopefully promote greater efforts in these areas and lead to better and more equitable healthcare for all.
by Stan Wolf
References:
Talks presented at the “AACR COVID-19 and Cancer” conference February 3-5, 2021:
- Financial hardship and mental health among cancer survivors during the Covid-19 pandemic: An analysis of the US Covid Impact Survey. Jessica Islam, UNC Lineberger Comprehensive Cancer Center
- Adolescent and young adult cancer patient and survivor employment changes during Covid-19 and associated financial toxicity. Austin Waters, Huntsman Cancer Institute
- Economic insurance challenges from the Covid-19 pandemic for individuals with cancer. Michael Halpern, National Cancer Institute
- Disparities in food insecurity among cancer survivors during the US Covid-19 pandemic. Marlene Camacho-Rivera, SUNY Downstate Health Sciences University