How is the drug name pronounced?
Brexucabtagene autoleucel: brek-suh-KAB-tuh-jeen aw-toh-LOO-sel
Tecartus: tek-ahr-tuhs
What cancer(s) does this drug treat?
Mantle cell lymphoma (MCL)
Tecartus is approved for:
- Patients with mantle cell lymphoma who have been previously treated, but whose cancer either did not respond to previous treatment (refractory disease) or responded but then came back (relapsed disease).
Acute lymphoblastic leukemia (ALL)
Tecartus is approved for:
- Patients with B-cell precursor acute lymphoblastic leukemia (ALL) whose cancer either did not respond to previous treatment (refractory disease) or responded, but then came back (relapsed disease).
Limitations of Use
Tecartus REMS program: Due to the risk of potentially serious side effects, Tecartus is currently only available through a Risk Evaluation and Mitigation Strategy (REMS) program. Hospitals or clinics that dispense Tecartus require certification for the program, ensuring proper monitoring and management of side effects associated with the drug.
Age: The safety and efficacy of Tecartus have not been established in patients under 18 years of age.
Fertility/Pregnancy/Breastfeeding: The effects of Tecartus on female and male fertility are not known. Tecartus is not recommended for women who are pregnant, and may pose a risk to a developing fetus. The risks associated with Tecartus during breastfeeding are not known, and risks to a breastfed infant cannot be excluded.
Effects on the ability to drive and use machines: Patients are advised to refrain from driving, engaging in hazardous occupations or activities, and operating heavy machinery for at least 8 weeks after receiving Tecartus.
What type of immunotherapy is this?
How does this drug work?
Target:
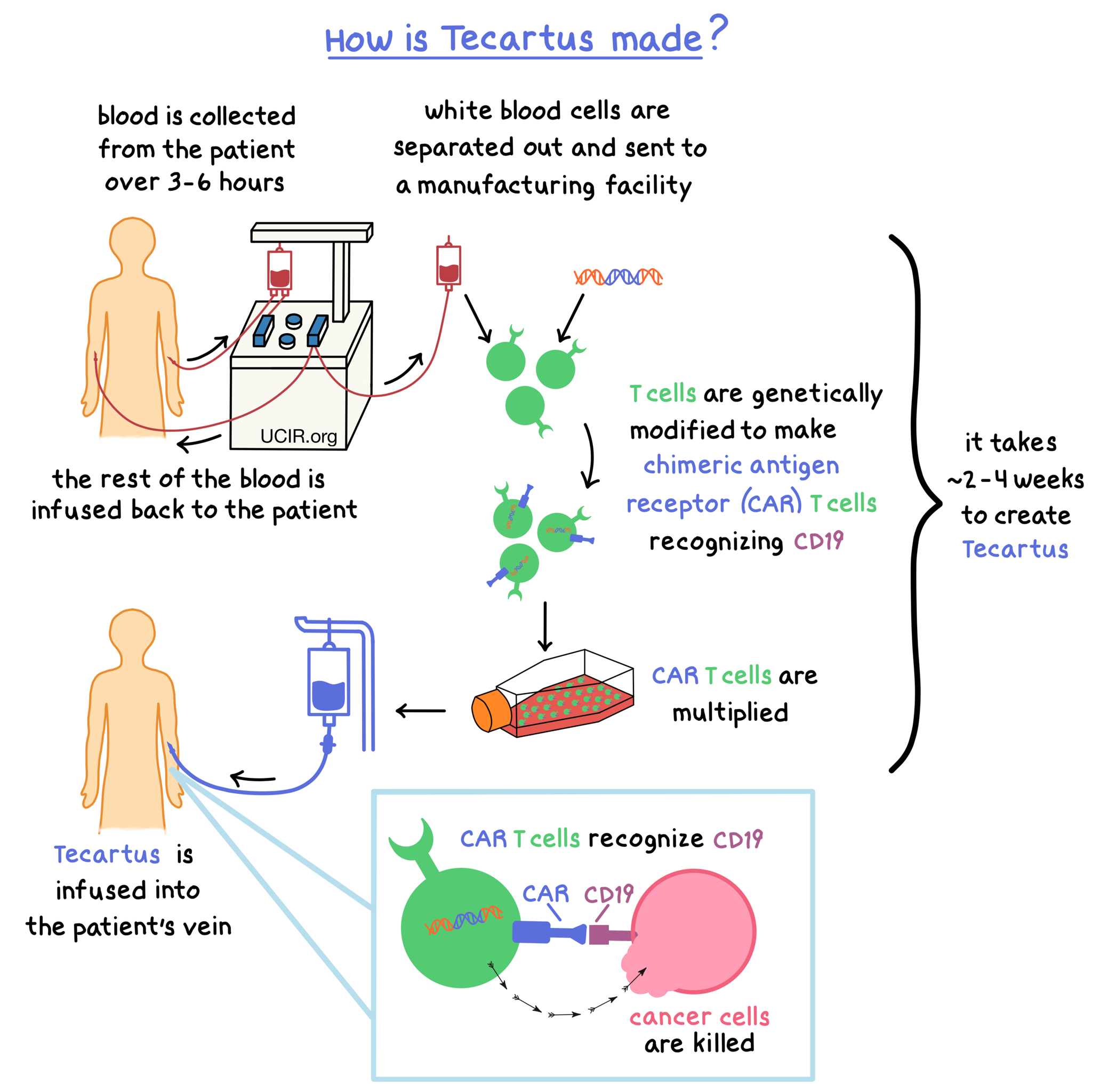
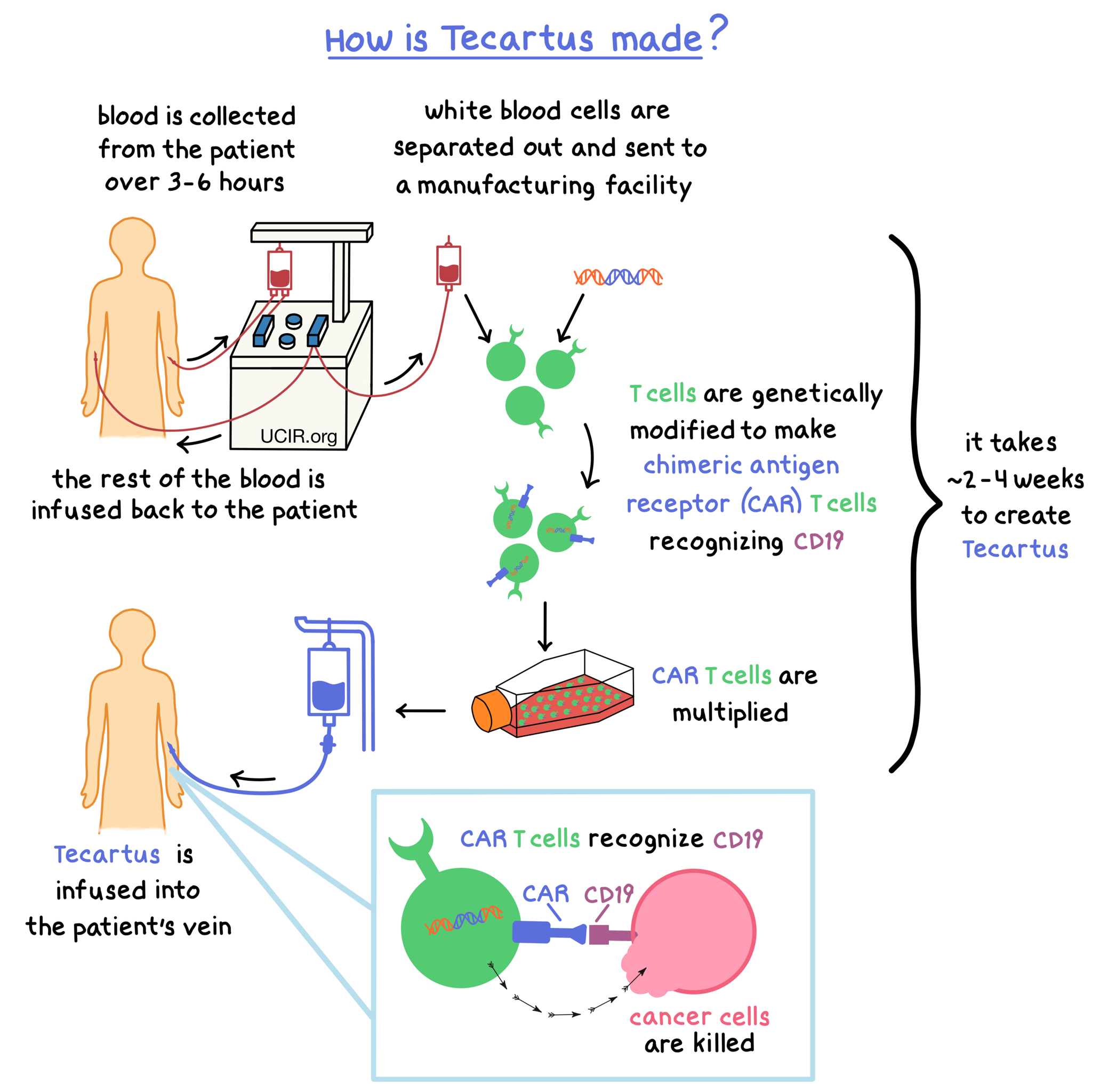
Tecartus is made from the patient’s own T cells (a type of white blood cell). In order to make Tecartus, blood is collected from the patient’s vein. In a process called leukapheresis, the white blood cells (including T cells) are separated from the collected blood, and the rest of the blood is returned to the patient; this process usually takes 3 to 6 hours and may need to be repeated. The collected white blood cells are sent to a specialized manufacturing facility where the patient’s T cells are genetically modified in such a way that they make a protein on their surface called chimeric antigen receptor (CAR). The modified T cells (“CAR T cells”) are multiplied to create millions of CAR T cells. The multiplied CAR T cells are then delivered back to the patient and are infused into the patient’s blood.
Once inside the body, The CARs on the surfaces of the modified CAR T cells can attach to a protein called CD19 on the surface of the cancer cells. When a CAR attaches to CD19, the T cells recognize the cancer cells and kill them. The entire process to create Tecartus, from collecting the blood to delivering the treatment, takes approximately 2 to 4 weeks.
How is this drug given to the patient?
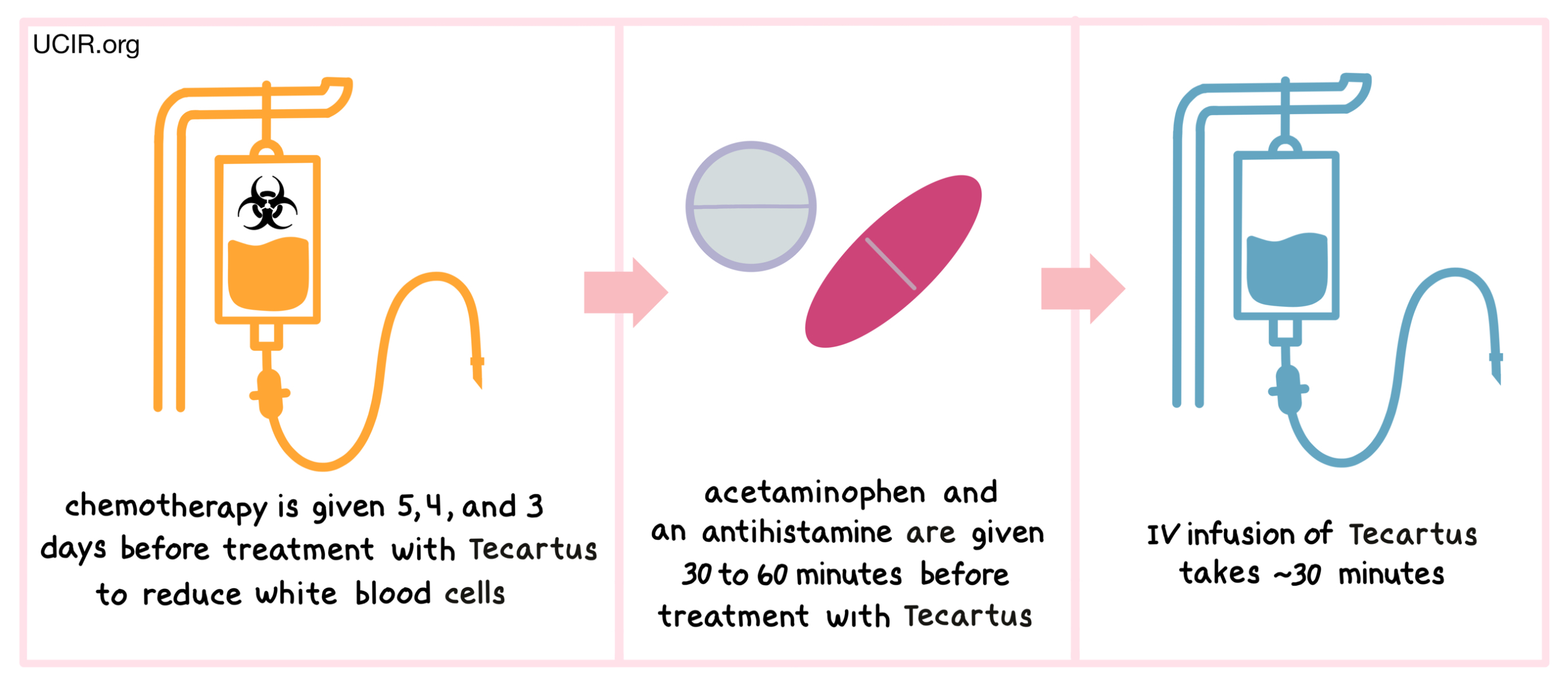
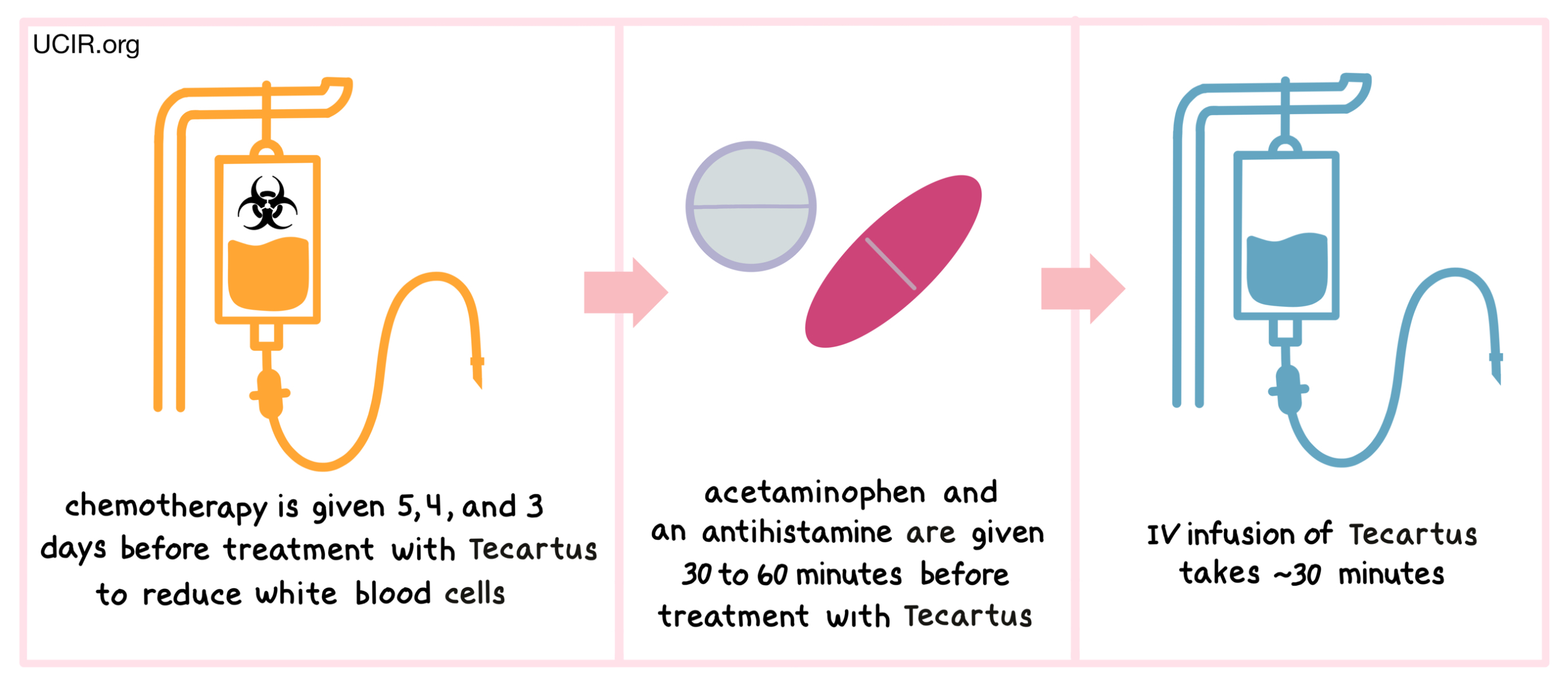
Before receiving Tecartus, patients are treated with a short course of chemotherapy to reduce the number of white blood cells. For patients with mantle cell lymphoma, tThe chemotherapies cyclophosphamide and fludarabine are administered 5, 4 and 3 days before treatment with Tecartus through a tube in the vein (intravenous, i.v.). For patients with acute lymphoblastic leukemia, fludarabine is administered on day -4, -3, and together with cyclophosphamide on day -2 before treatment with Tecartus through an intravenous infusion. The reduction in the patient’s white blood cell count gives the CAR T cells in Tecartus enough space to multiply, and provides them with the resources needed to survive longer in the patient. About 30 to 60 minutes before receiving Tecartus, patients receive acetaminophen and an antihistamine to reduce the chance of reactions to the infusion.
Patients receive Tecartus through an intravenous infusion. The administration of Tecartus usually takes about 30 minutes.
Patients should plan to stay close to the treatment location for at least 4 weeks after receiving Tecartus and will be monitored daily for at least 7 days following administration of Tecartus.
What are the observed clinical results?
It is important to keep in mind that each patient’s actual outcome is individual and may be different from the results found in the clinical studies. In addition, with immunotherapy, sometimes it takes several months for responses to be observed. The long-term clinical trial data currently available is limited, and more clinical trials are ongoing.
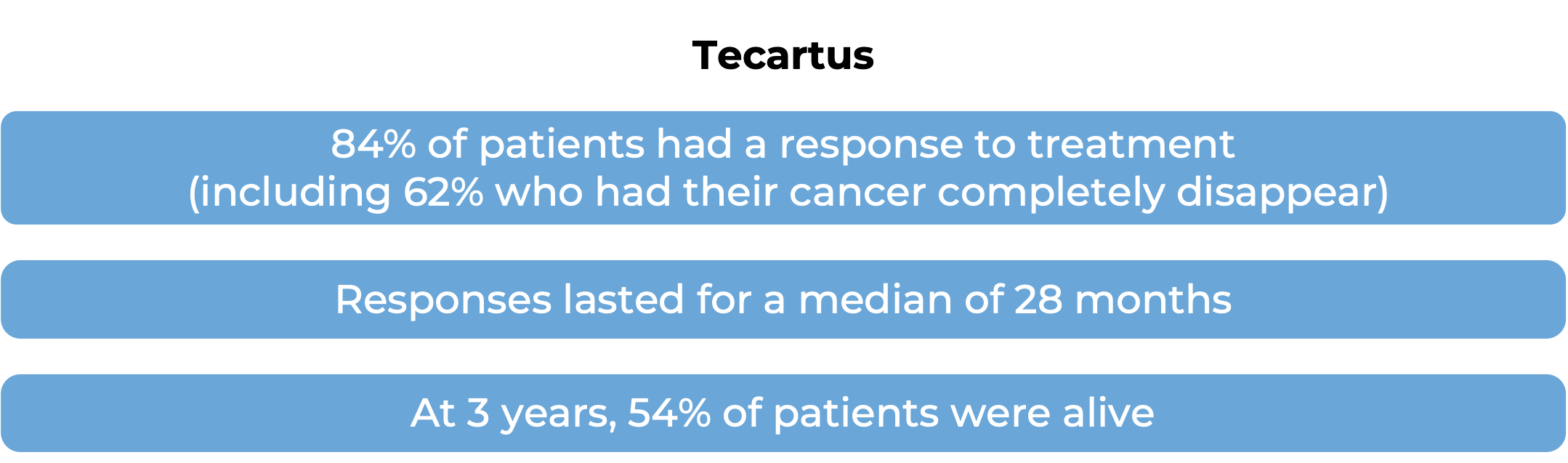
Mantle cell lymphoma
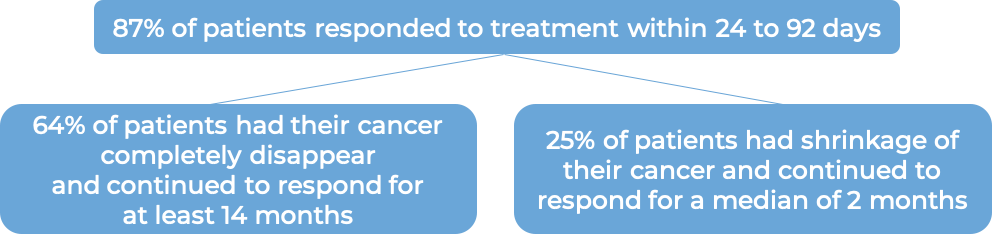
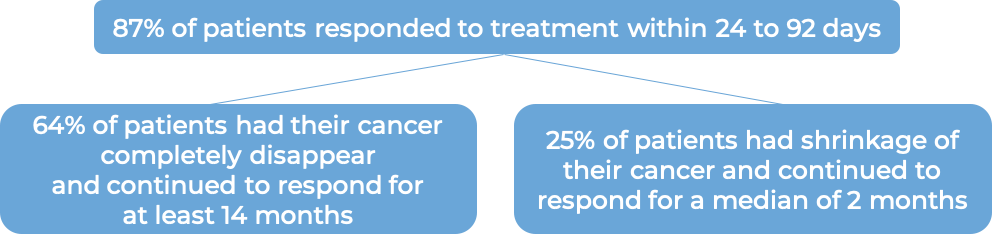
In a clinical trial, 60 patients with mantle cell lymphoma who had been previously treated, but whose cancer either did not respond (refractory) or had since returned (relapsed), were treated with a single infusion of Tecartus.
Acute lymphoblastic leukemia (ALL)
In a clinical trial, 54 patients with B-cell precursor acute lymphoblastic leukemia (ALL) whose cancer either did not respond to previous treatment (refractory disease) or responded, but then came back (relapsed disease), were treated with a single infusion of Tecartus. 52% of patients had their cancer completely disappear within 3 months, and based on incoming results, it has been estimated that more than half of these patients will stay cancer-free for more than 12 months.
What are the potential side effects?
Most patients receiving Tecartus experience side effects. Some side effects, such as cytokine release syndrome (CRS), neurological toxicities, and hemophagocytic lymphohistiocytosis/macrophage activation syndrome (HLH/MAS), may be severe or life-threatening. Patients will be monitored daily by their health care provider for at least 7 days after the infusion of Tecartus, and should remain within a reachable distance of the healthcare facility for at least four weeks. Patients and caregivers receive careful instructions to monitor for signs and symptoms related to CRS and neurological toxicities. Both conditions are managed by the health care provider.
Cytokine release syndrome (CRS)
CRS is caused by a widespread release of molecules called cytokines, which are involved in inflammation and can affect the function of various organs. Cytokines may be released by the CAR T cells in Tecartus or by other immune cells in the patient’s body. Symptoms of CRS include high fever, chills, difficulty breathing, severe muscle or joint pain, severe nausea, vomiting, diarrhea, very low blood pressure, and dizziness or lightheadedness. CRS typically occurs between 1 and 10 days after a Tecartus infusion, and the health care provider should be immediately notified if symptoms occur.
Neurological toxicities
Some of the cytokines released during CRS can result in disruption of the blood–brain barrier, leading to the development of neurological toxicities. Symptoms of neurological toxicities include confusion, altered or decreased consciousness, seizures, loss of balance, and difficulty speaking and understanding. Neurological toxicities typically occur about 7 days after a Tecartus infusion, but could occur up to 8 weeks or later after the infusion.
Hemophagocytic lymphohistiocytosis/Macrophage activation syndrome (HLH/MAS)
Some of the cytokines released during cytokine release syndrome can result in an excessive activation of the immune system, causing HLH/MAS. In HLH/MAS, immune cells such as lymphocytes (in HLH) and macrophages (in MAS) begin attacking and destroying healthy tissues, causing widespread tissue damage and inflammation. Symptoms of HLH/MAS typically occur within 8-9 days of receiving Tecartus and include low blood pressure, low oxygen levels in the blood, altered organ function, and multiple organ failure.
Other side effects
Tecartus can lead to other side effects, some of which could be long lasting. The CAR T cells in Tecartus kill cancer cells that have the molecule CD19 on their surface; however, CD19 is also found on the surface of healthy B cells, which can also be killed by Tecartus. The decrease in healthy B cells leads to low levels of antibodies (immunoglobulins) and an increased risk of serious, potentially life-threatening, infections. If a patient is a carrier of the hepatitis B virus, Tecartus can cause serious liver problems, including liver failure and death. Other possible side effects include nausea, diarrhea, fever, low blood pressure, fast heartbeat, headache, muscle pain, lower back pain, sleepiness, confusion, temporary memory and coordination problems, low blood cell counts, serious allergic reactions, and development of other cancers.
For a more complete list of possible side effects, see the full prescribing information.
Manufacturer
Kite Pharma
Approval
FDA and EMA
Link to drug website
Last update on October 6, 2021
How is the drug name pronounced?
What cancer(s) does this drug treat?
Mantle cell lymphoma (MCL)
Tecartus is approved for:
- Patients with mantle cell lymphoma who have been previously treated with at least two different types of therapy, including a BTK inhibitor, but whose cancer either did not respond to previous treatment (refractory disease) or responded, but then came back (relapsed disease).
Acute lymphoblastic leukemia (ALL)
Tecartus is approved for:
- Adult patients (26 years of age and older) with B-cell precursor acute lymphoblastic leukemia (ALL) whose cancer either did not respond to previous treatment (refractory disease) or responded, but then came back (relapsed disease).
Limitations of Use
Limitations: Tecartus should only be administered in a qualified treatment center and by adequately trained healthcare professionals who can ensure proper monitoring and immediate management of side effects associated with the drug.
Age: The safety and efficacy of Tecartus have not been established in patients under 18 years of age.
Fertility/Pregnancy/Breastfeeding: The effects of Tecartus on female and male fertility are not known. Tecartus is not recommended for women who are pregnant, and may pose a risk to a developing fetus. The risks associated with Tecartus during breastfeeding are not known, and risks to a breastfed infant cannot be excluded.
Exclusions: The benefits and risks of treatment with Tecartus in patients with active hepatitis B virus (HBV), hepatitis C virus (HCV), or human immunodeficiency virus (HIV) infection have not been established. The benefits and risks of treatment with Tecartus in patients with lymphoma that has formed in or spread to the brain or spinal cord have not been established. Tecartus is not recommended for patients who have received a stem cell transplant and suffer from graft-versus-host disease.
Vaccinations: Live virus vaccinations (e.g., chickenpox or measles, mumps, and rubella (MMR)) are not recommended for at least 7 weeks prior to or during Tecartus treatment, and until the patient's white blood cell count has recovered following treatment.
Effects on the ability to drive and use machines: Patients are advised to refrain from driving, engaging in hazardous occupations or activities, and operating heavy machinery for at least 8 weeks after receiving Tecartus.
What type of immunotherapy is this?
How does this drug work?
Target:
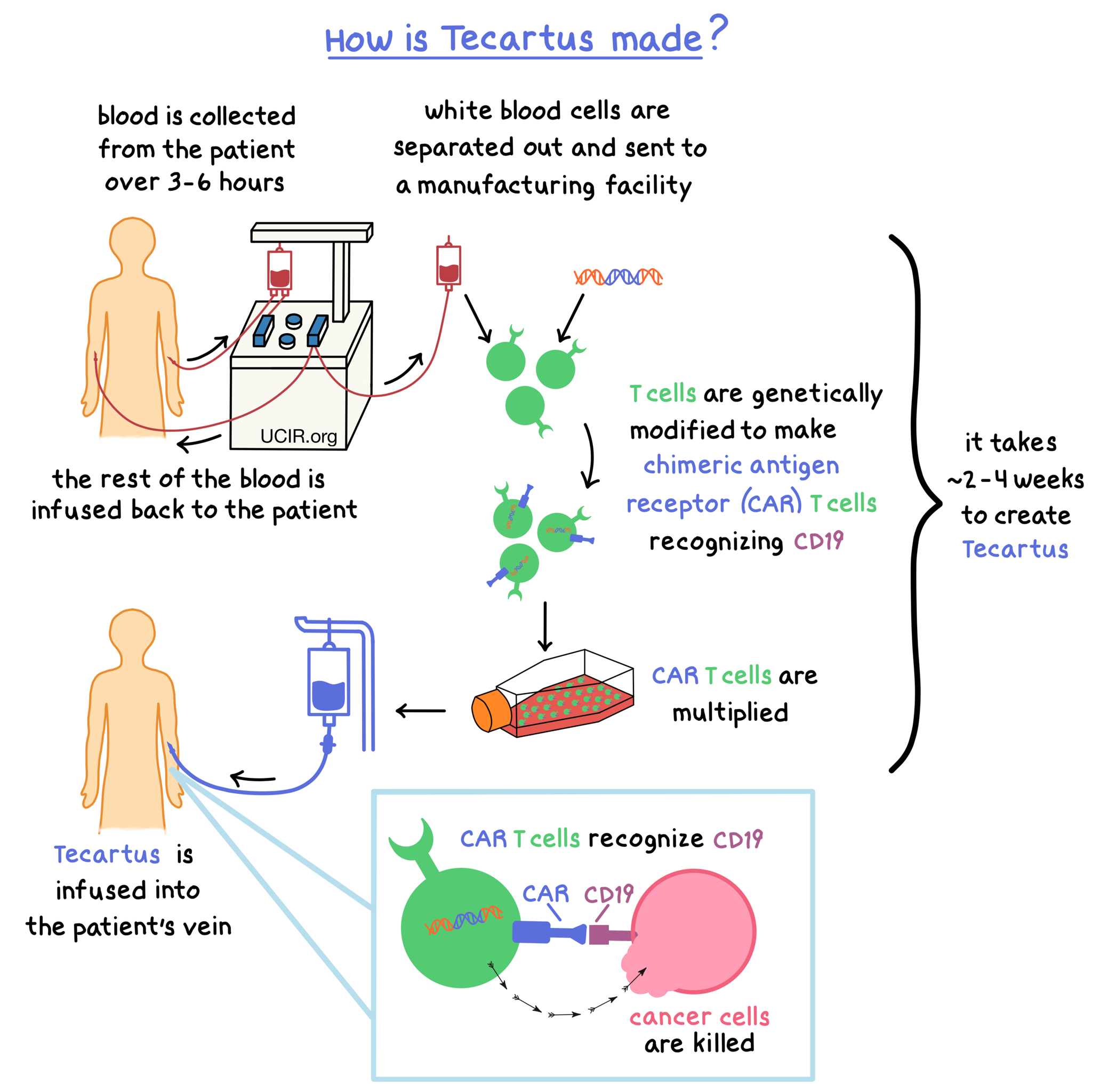
Tecartus is made from the patient’s own T cells (a type of white blood cell). In order to make Tecartus, blood is collected from the patient’s vein. In a process called leukapheresis, the white blood cells (including T cells) are separated from the collected blood, and the rest of the blood is returned to the patient; this process usually takes 3 to 6 hours and may need to be repeated. The collected white blood cells are sent to a specialized manufacturing facility where the patient’s T cells are genetically modified in such a way that they make a protein on their surface called chimeric antigen receptor (CAR). The modified T cells (“CAR T cells”) are multiplied to create millions of CAR T cells. The multiplied CAR T cells are then delivered back to the patient and are infused into the patient’s blood.
Once inside the body, The CARs on the surfaces of the modified CAR T cells can attach to a protein called CD19 on the surface of the cancer cells. When a CAR attaches to CD19, the T cells recognize the cancer cells and kill them. The entire process to create Tecartus, from collecting the blood to delivering the treatment, takes approximately 2 to 4 weeks.
How is this drug given to the patient?
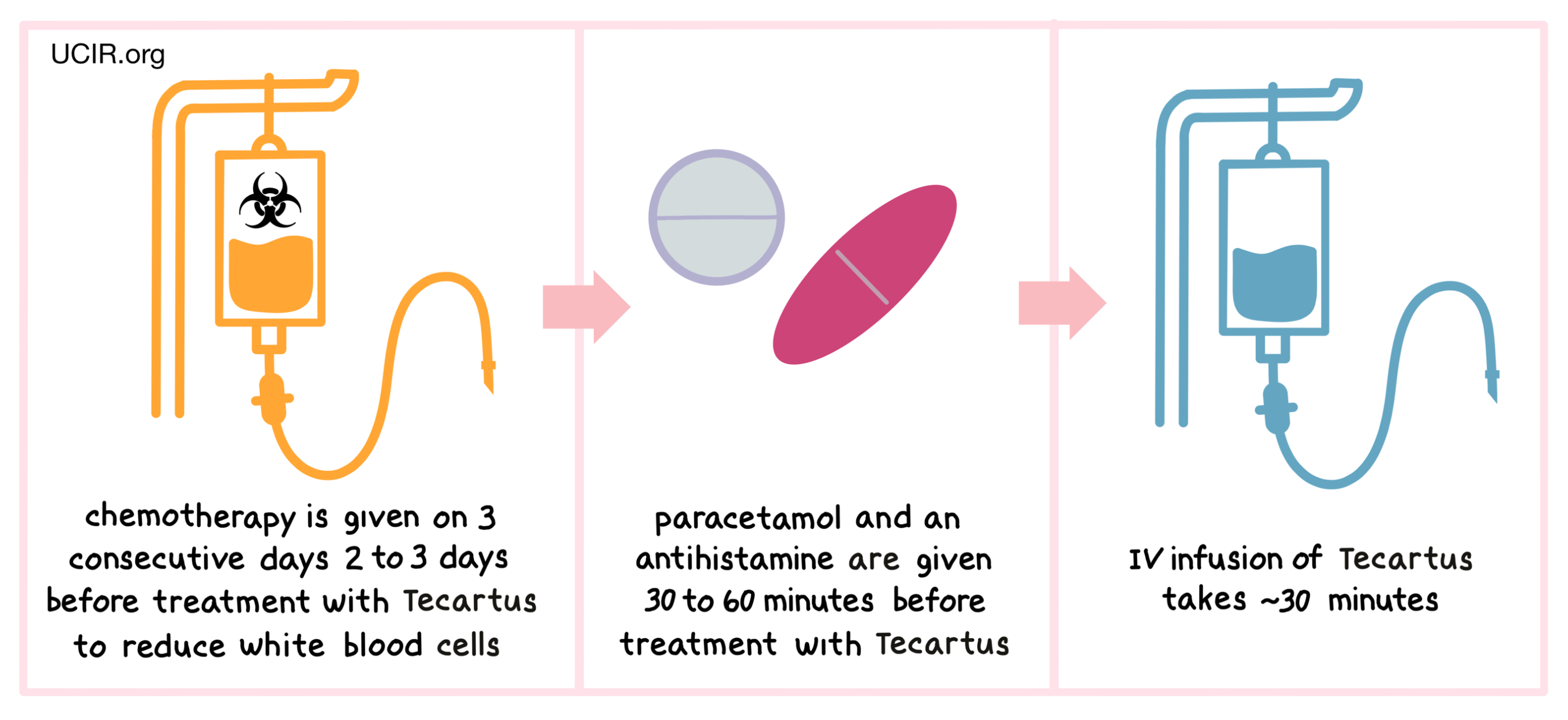
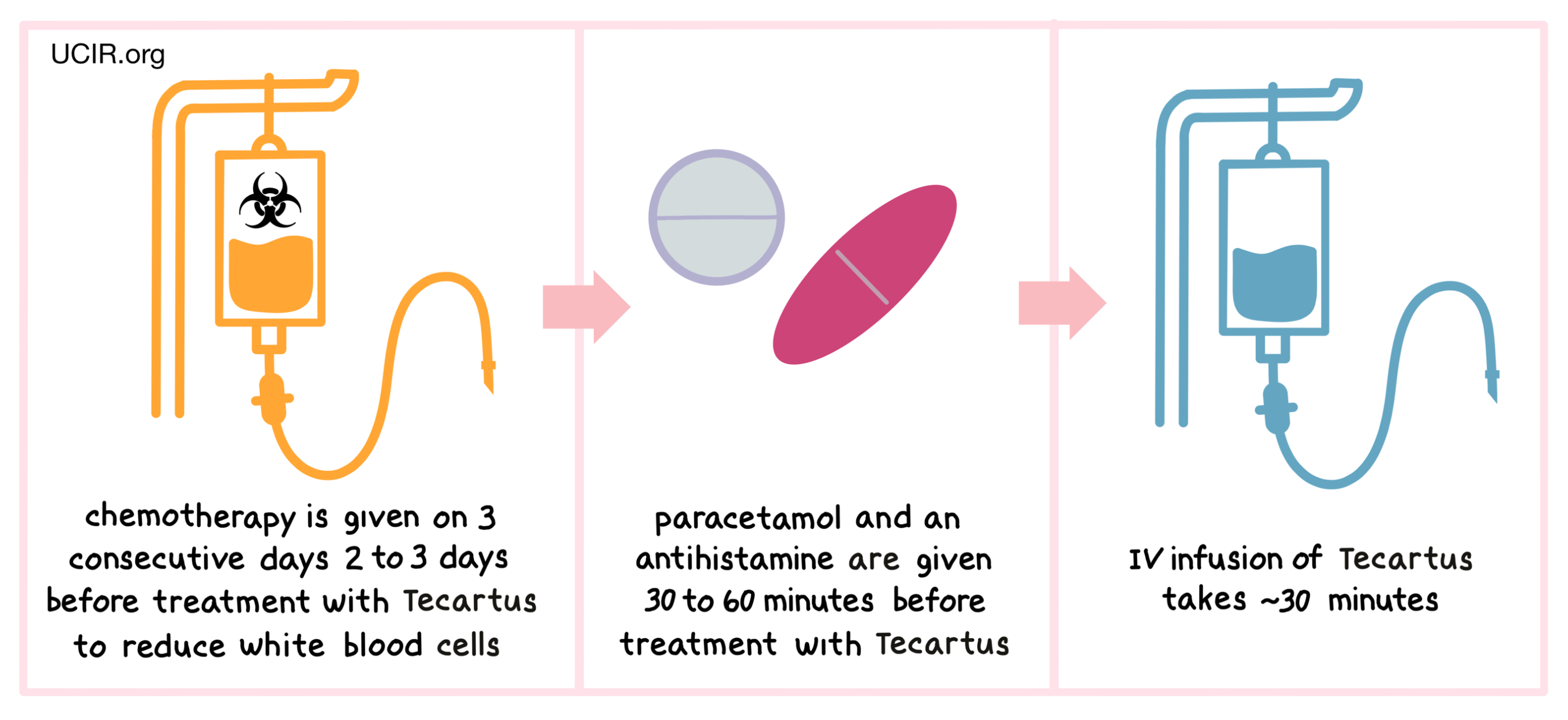
Before receiving Tecartus, patients are treated with a short course of chemotherapy to reduce the number of white blood cells in their body. The reduction in white blood cell count helps make room in the blood for the CAR T cells in Tecartus to multiply, and ensures that there are enough resources for them to survive in the patient. The chemotherapies cyclophosphamide and/or fludarabine are administered on three consecutive days 2 to 3 days before treatment with Tecartus, through a tube in the vein (intravenous, i.v.). About 30 to 60 minutes before receiving Tecartus, patients receive paracetamol and an antihistamine to reduce the chance of reactions to the infusion.
Patients receive Tecartus through an intravenous (i.v.) infusion (through a tube in the vein). The administration of Tecartus usually takes about 30 minutes.
Patients may be required to stay in the hospital for the first 10 days following administration of Tecartus and are monitored daily. Thereafter, patients should plan to stay close to the treatment location for at least 4 weeks after receiving Tecartus.
What are the observed clinical results?
It is important to keep in mind that each patient’s actual outcome is individual and may be different from the results found in the clinical studies. In addition, with immunotherapy, sometimes it takes several months for responses to be observed. The long-term clinical trial data currently available is limited, and more clinical trials are ongoing.
Mantle cell lymphoma
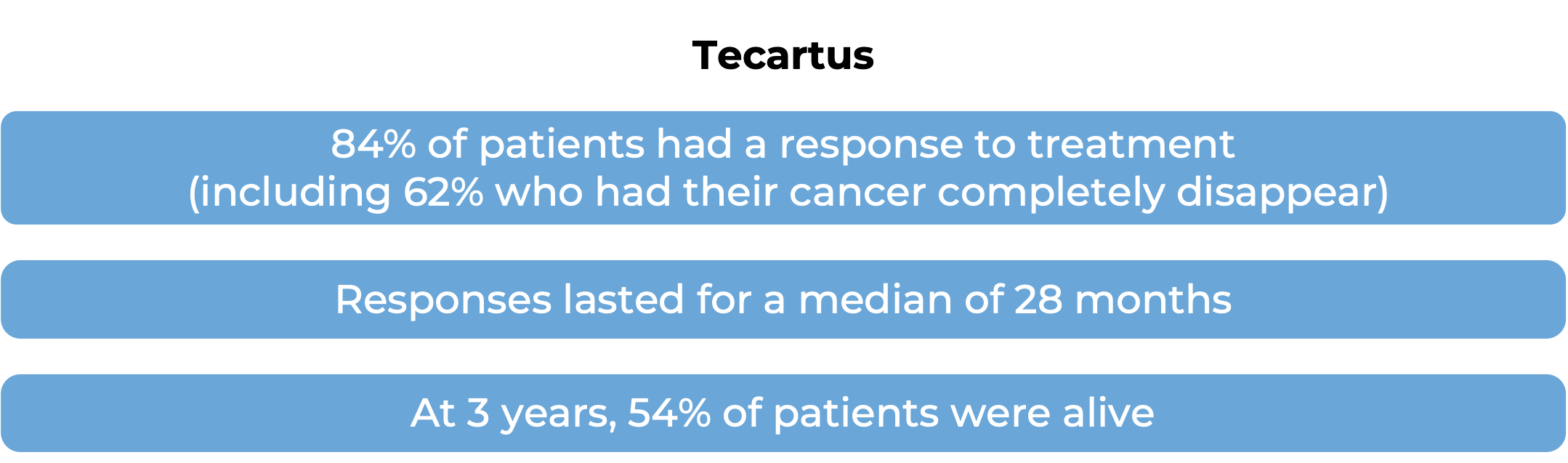
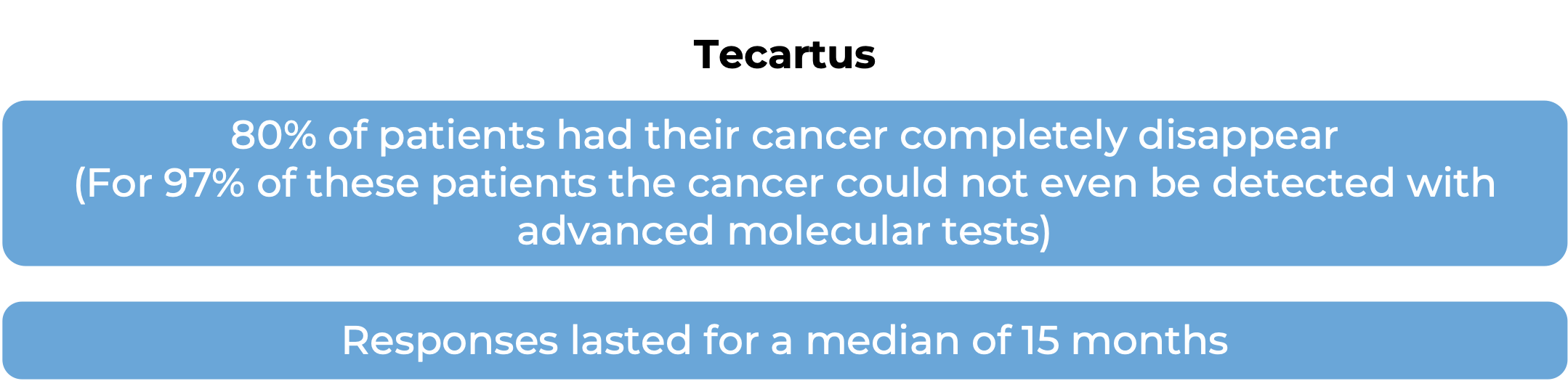
In a clinical trial, 68 of 74 patients with mantle cell lymphoma who had been previously treated, but whose cancer either did not respond (refractory) or had since returned (relapsed), were treated with a single infusion of Tecartus. Among all 74 patients, at a median follow-up of 3 years (37 months):
In this clinical trial, the median time between blood collection and the final Tecartus product was 13 days, and between blood collection and administration of Tecartus was 27 days.
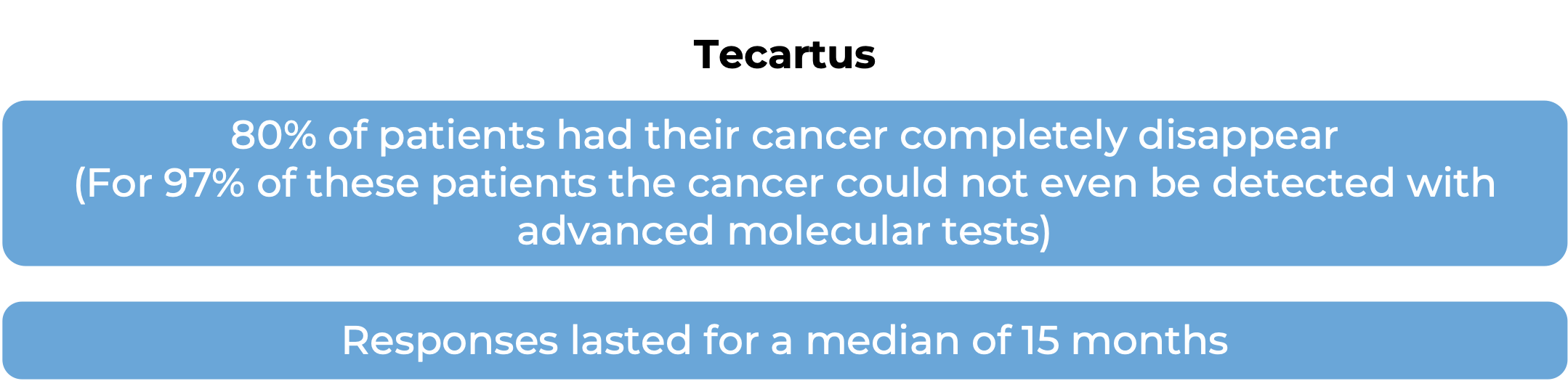
Acute lymphoblastic leukemia (ALL)
In a clinical trial, 55 patients with B-cell precursor acute lymphoblastic leukemia (ALL) whose cancer either did not respond to previous treatment or responded, but then came back, were treated with Tecartus. At median follow-up of 21 to 24 months:
In this clinical trial, the median time between blood collection and the final Tecartus product was 16 days, and between blood collection and administration of Tecartus was 29 days. Responses to treatment were observed 1 to 3 months after Tecartus was given.
What are the potential side effects?
Most patients receiving Tecartus experience side effects. Some side effects, such as cytokine release syndrome (CRS) and neurological toxicities, may be severe or life-threatening. Patients are monitored daily by their health care provider for at least 10 days after the infusion of Tecartus, and should remain within a reachable distance of the healthcare facility for at least four weeks. Patients and caregivers receive careful instructions to monitor for signs and symptoms related to CRS and neurological toxicities. Both conditions are managed by the health care provider.
Cytokine release syndrome (CRS)
CRS is caused by a widespread release of molecules called cytokines, which are involved in inflammation and can affect the function of various organs. Cytokines may be released by the CAR T cells in Tecartus or by other immune cells in the patient’s body. Symptoms of CRS include high fever, chills, difficulty breathing, severe muscle or joint pain, severe nausea, vomiting, diarrhea, very low blood pressure, and dizziness or lightheadedness. CRS typically occurs between 1 and 10 days after a Tecartus infusion, and the health care provider should be immediately notified if symptoms occur. 91% of patients treated with Tecartus experience CRS.
Neurological toxicities
Some of the cytokines released during CRS can result in disruption of the blood–brain barrier, leading to the development of neurological toxicities. Symptoms of neurological toxicities include confusion, altered or decreased consciousness, seizures, loss of balance, and difficulty speaking and understanding. Neurological toxicities typically occur about 8 days after a Tecartus infusion, but could occur up to 8 months after the infusion.
Other side effects
Tecartus can lead to other side effects, some of which could be long lasting. The CAR T cells in Tecartus kill cancer cells that have the molecule CD19 on their surface; however, CD19 is also found on the surface of healthy B cells, which can also be killed by Tecartus. The decrease in healthy B cells leads to low levels of antibodies (immunoglobulins) and an increased risk of serious, potentially life-threatening, infections. If a patient is a carrier of the hepatitis B virus, Tecartus can cause serious liver problems, including liver failure and death. Other possible side effects include fatigue, nausea, diarrhea, fever, low blood pressure, fast or slow heartbeat, headache, muscle pain, lower back pain, sleepiness, confusion, temporary memory and coordination problems, low blood cell counts, and serious allergic reactions.
For a more complete list of possible side effects, see the full prescribing information.
Manufacturer
Kite Pharma
Approval
FDA and EMA
Link to drug website
Last update on February 8, 2023