Approval in the US
The US product name for Qarziba is Unituxin.
How is the drug name pronounced?
Qarziba: Car-ZEE-buh
Dinutuximab beta: Dee-noo-TUX-uh-mab bey-tuh
What cancer(s) does this drug treat?
Neuroblastoma
Qarziba is approved for:
- Pediatric patients age 12 months and older with neuroblastoma, who have had at least a partial response to prior treatment with chemotherapy, followed by myeloablative therapy and stem cell transplant, or whose cancer came back (relapsed) or did not respond to treatment (refractory) in the past, and who are now at a high risk for the cancer to come back or get worse. Patients with actively progressing disease should be treated with other measures first to stabilize the disease. For patients with relapsed or refractory neuroblastoma, or partial response to the first therapy, Qarziba is used in combination with an IL-2 cytokine drug (e.g., Proleukin).
Limitations of Use
Age: Qarziba is approved for use in pediatric patients 12 months or older.
Pregnancy/Breastfeeding: The risks associated with Qarziba during pregnancy are not known and cannot be ruled out. Due to the potential for harm to the fetus, Qarziba is not recommended for use during pregnancy. Patients who could become pregnant are advised to use contraception during treatment and for 6 months after the last dose of Qarziba. The risks associated with Qarziba during breastfeeding are not known and cannot be ruled out. Due to the potential for negative reactions in the breastfed child, women are advised not to breastfeed during treatment with Qarziba and for 6 months after the last dose of Qarziba.
Corticosteroids: Treatment with corticosteroids is not recommended within 2 weeks prior to the first dose of Qarziba and for at least 1 week after the last treatment course with Qarziba (except for life-threatening conditions), as they can suppress the immune system.
Vaccinations: Vaccinations should be avoided during administration of dinutuximab beta until 10 weeks after the last treatment course, as they may increase the risk for neurological toxicities.
Intravenous immunoglobulin: The use of intravenous immunoglobulins is not recommended during treatment with Qarziba, as they may interfere with Qarziba’s cancer-killing functions.
Effects on the ability to drive and use machines: Patients are advised to refrain from driving, engaging in hazardous occupations or activities, and operating heavy machinery during treatment with Qarziba.
What type of immunotherapy is this?
- Cell-killing antibody
How does this drug work?
Target:
- GD2
Qarziba is an antibody that was made in a laboratory and designed to attach to a protein molecule called GD2. GD2 is present on the surface of nerve cells, but is present in much higher quantities on the surface of neuroblastoma cells. Higher-than-normal amounts of GD2 on neuroblastoma cells make these cells the main targets of Qarziba.
Qarziba and other antibody molecules have an overall “Y” shape. The two tips of the upper arms of the “Y” shape are the parts of the antibody that can very precisely bind to their targets. For Qarziba, the tips of the upper arms bind to GD2. The stem of Qarziba “Y” shape has binding sites for immune cells or other parts of the immune system.
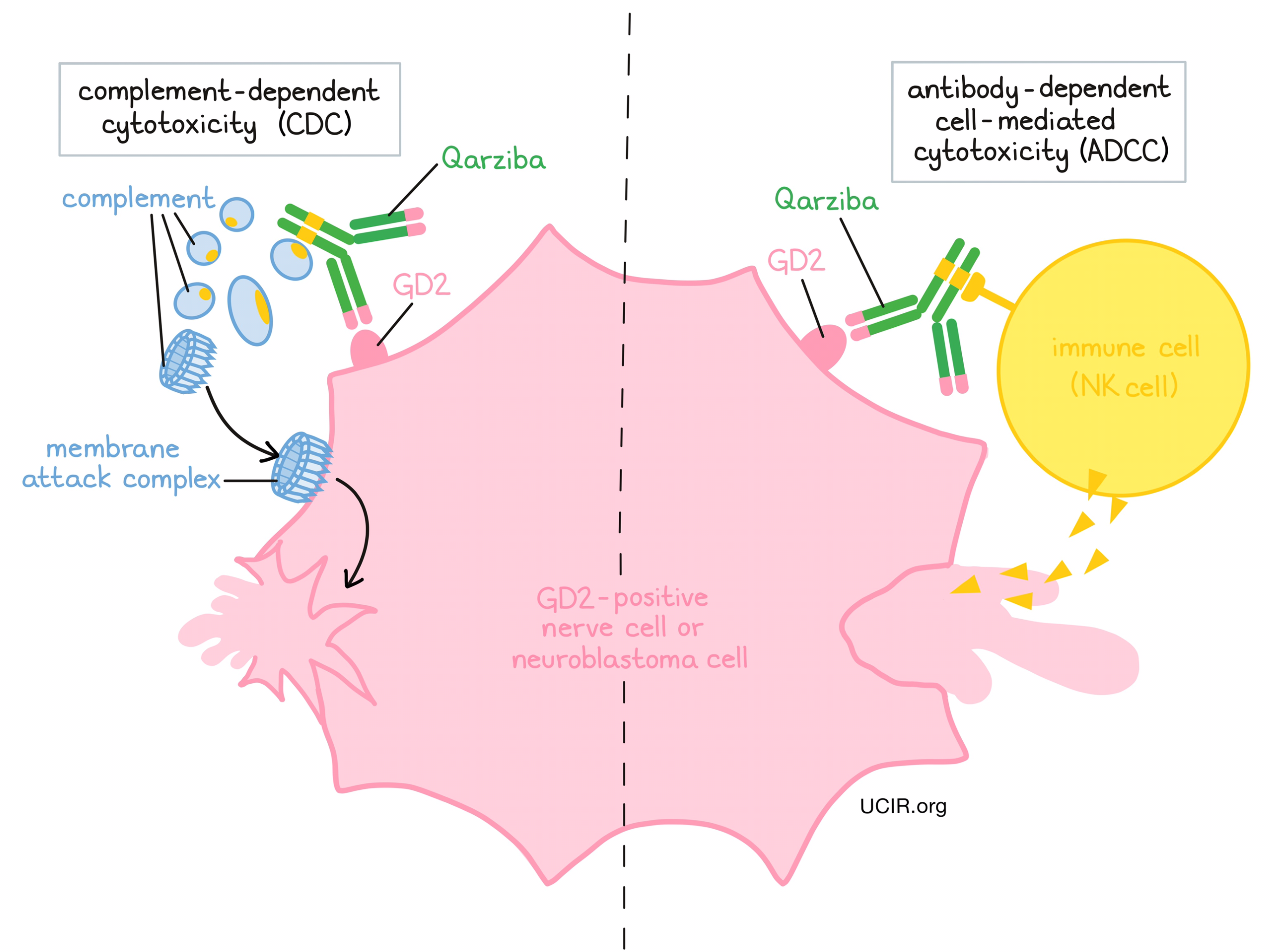
Qarziba works to kill cancer cells in at least two ways:
Complement-dependent cytotoxicity (CDC)
When bound to GD2 on the surface of neuroblastoma cells, the stem of Qarziba can attract and bind molecules of the immune system called “complement” that freely flow in the blood or tissues. Activation of the complement system causes the formation of the “membrane attack complex”, which can puncture and destroy the cell that Qarziba is bound to.
Antibody-dependent cell-mediated cytotoxicity (ADCC)
When bound to GD2 on the surface of neuroblastoma cells, the stem of Qarziba can also attract and bind immune cells (like NK cells). This allows Qarziba to act as a bridge between the target cell and the immune cell. The immune cell then releases molecules that can kill the cell Qarziba is bound to.
How is this drug given to the patient?
Treatment with Qarziba requires a hospital stay. Qarziba is given over the course of five 35-day treatment cycles. Qarziba is administered slowly through a tube in the vein (intravenous infusion, or i.v.). It can either be given continuously at a lower dose over the first 10 days of each cycle, or a stronger dose can be given as five daily infusions over the course of 8 hours each day for the first 5 days of each treatment cycle. When IL-2 is used in combination with Qarziba, it is given via an injection under the skin. IL-2 is given for 5 days in a row starting 7 days before the first dose of Qarziba, and then for another 5 days in a row starting at the same time as Qarziba treatment.
To manage possible risks and side effects associated with Qarziba, patients receive several pain management medications, starting 3 days prior to treatment with Qarziba. About 20 minutes prior to each infusion of Qarziba and periodically throughout the treatment, patients also receive antihistamines to prevent allergic reactions. During treatment with Qarziba, patients are closely monitored for reactions to the infusion. If symptoms of an infusion-related reaction occur, the infusion may be slowed or entirely stopped, and additional medications may be required, depending on the severity of the reaction.
What are the observed clinical results?
It is important to keep in mind that each patient’s actual outcome is individual and may be different from the results found in the clinical studies. In addition, with immunotherapy, sometimes it takes several months for responses to be observed.
Neuroblastoma, relapsed/refractory
In a compassionate use study and later a clinical trial, 98 patients with neuroblastoma that had either failed to respond to treatment (refractory) or had responded to treatment, but their cancer had since come back (relapsed), were treated with Qarziba plus IL-2 and 13-cis-RA. Patients ranged in age from 1 to 26 years old and had previously been treated with chemotherapy followed by autologous stem cell transplantation; radiotherapy; and/or surgery. Overall, 36% of patients who had evidence of disease at the start of treatment responded. Patients who had refractory disease were more likely to respond than those with relapsed disease (41% vs 29%). After two years, 70% and 78% of patients with refractory disease were alive in the compassionate use study and the clinical trial, respectively, compared to 69% and 42% of patients with relapsed disease.
Neuroblastoma, previously treated with autologous stem cell transplantation
In a clinical study, 370 patients who had achieved at least a partial response after chemotherapy and were then treated with myeloablative therapy and autologous stem cell transplantation were treated with Qarziba plus cis-13-RA with or without IL-2. Patients ranged in age from 0.6 to 20 years old. In the 211 patients without evidence of disease at the start of treatment, 71 to 72% were alive after 3 years, and the addition of IL-2 had no effect on outcome. In the 149 patients with evidence of disease at the start of treatment, 54% of patients who received Qarziba without IL-2 and 63% of patients who received Qarziba with IL-2 were alive after 3 years.
What are the potential side effects?
The most common side effects of Qarziba include rapid swelling of arms, legs and other body parts; rapid drops in blood pressure; light-headedness; breathing difficulties (capillary leak syndrome); pain in the stomach, throat, chest, face, hands, feet, legs, arms, back, neck, joint, or muscles; allergic reactions and cytokine release syndrome, with symptoms such as face or throat swelling; dizziness; hives; rapid or noticeable heartbeat; low blood pressure; rash; fever; nausea; chills; vomiting; diarrhea; constipation; inflammation of the mouth and lips; cough; itching, oxygen deficiency; tissue swelling (in the face, lip, around the eye, in the lower limbs); increased weight; infection, in particular infection associated with the catheter that delivers the medicine; headache; dilated pupils or abnormal pupil reactions; abnormal blood or urine tests (blood cells and other components, liver function, renal function). Other common side effects include life-threatening infections (sepsis); fits; agitation; anxiety; nerve disorder in the arms and/or legs (with abnormal sensations or weakness); light-headedness; trembling; muscle spasms; paralysis of eye muscles, blurred vision, light sensitivity, or swelling in the retina; high blood pressure; cardiac failure, or fluid around the heart; respiratory failure or fluid in the lungs; sudden constriction of the airways (bronchospasm, laryngospasm); rapid breathing; decreased appetite; abdominal distension; accumulation of fluid in the abdominal cavity; injection-site reactions, including skin problems such as reddening, dry skin, eczema, or excessive sweating; reaction to light; an inability to pass urine or reduced urine volume; decreased weight associated with loss of fluids.
Some side effects and reactions associated with Qarziba can be severe or life-threatening. Patients are monitored for signs and symptoms related to these conditions throughout treatment and should report any symptoms immediately. These conditions are managed by the healthcare provider.
Infusion-related reactions
Infusion-related reactions are an adverse response to receiving an infusion. Almost all patients treated with Qarziba experience infusion-related reactions with some level of severity. Most of these reactions typically occur within 24 hours of the first or second infusion. Symptoms include hives (itchy red welts) or rash, itchiness (pruritus), and swelling of the tongue, lips, face, or throat. Coughing, shortness of breath, wheezing, difficulty breathing, weakness, low blood pressure, dizziness, or faintness can also occur. Palpitations (feeling as if your heart is fluttering or racing) and chest pain can also be symptoms of a reaction. Serious reactions include anaphylactic shock and cardiac arrest (the heart stops pumping blood around the body).
Nerve damage
Because Qarziba can also target the GD2 molecule on nerve cells, treatment with Qarziba may result in damage to the nervous system, resulting in:
- Pain - most patients treated with Qarziba experienced bodily pain with some degree of severity, including pain in the stomach region, bones, neck, arms, and legs.
- Transverse myelitis - an inflammation of the spinal cord. Symptoms include pain, weakness, sensory problems (numbness, tingling, burning, or aversion to light, sound, touch, taste, or smell), and bladder or bowel problems.
- Reversible posterior leukoencephalopathy syndrome - caused by swelling in the brain that does not compromise blood flow. Symptoms of RPLS include high blood pressure, headache, seizures, visual disturbances, and altered consciousness.
- Peripheral neuropathy - caused by damage to nerves that are responsible for relaying sensory and motor information. Symptoms of peripheral neuropathy include pain, a persistent “pins and needles” sensation, tingling, chilling, burning, numbness, and weakness.
- Neurological disorders of the eye - Symptoms include unequal pupils, blurred or bad vision, difficulty focusing vision, dilated pupils, and extreme light sensitivity.
- Prolonged urinary retention - a condition in which patients cannot completely empty the bladder when peeing. If this condition does not resolve after the administration of opioids has been stopped, then treatment with Qarziba should be permanently stopped.
Low blood pressure
Low blood pressure is a common side effect of treatment with Qarziba, however in rare cases, the condition can become serious. Patients receive iv, hydration and have their blood pressure monitored during each infusion with Qarziba to monitor for any signs and symptoms of low blood pressure.
Patients should report any symptoms to their healthcare provider, who can then initiate actions to limit or reverse the side effects. Treatment with Qarziba may be interrupted and later resumed at a lower dose, or discontinued entirely depending on the severity of the condition. For a more complete list of possible side effects, see the full prescribing information.
Additional Information
Manufacturer
Rentschler Biopharma SE Patheon Italia S.P.A.
Approval
EMA and FDA (US product name: Unituxin)
Links to drug websites
- US: https://www.unituxin.com/
- Europe: https://www.ema.europa.eu/en/medicines/human/EPAR/qarziba-previously-dinutuximab-beta-eusa-dinutuximab-beta-apeiron
Last updated: December 22, 2023


