Patient 3737: An Early Story of Success in Cancer Immunotherapy
2019-12-26

At the age of 41, Melinda Bachini was diagnosed with widely metastatic cholangiocarcinoma, a rare cancer that begins in the bile ducts. Immediately after diagnosis, she underwent surgery to remove the cancer, and while the doctors thought they had gotten it all, Melinda’s cancer soon reappeared in her lungs. She began a series of standard-of-care chemotherapy regimens – none of which were expected to be curative – and one by one, each chemotherapy regimen became too toxic to bear. Melinda knew that a clinical trial was the only chance she had at actually beating her cancer, but every trial she saw was just a different combination of the same old chemo. Maxed out on the toxicities of chemotherapy, Melinda stopped treatment. Her tumors grew and she developed a chronic cough as many tumors lined her lungs. She could barely walk up stairs, laugh, or even be hugged too tightly without spiraling into violent coughing fits. Just when it seemed like her options had run dry, Melinda spotted a new kind of clinical trial.
Led by Dr. Steven Rosenberg, MD and run by Dr. Eric Tran, PhD, this clinical trial was for a then up-and-coming immunotherapy known as tumor-infiltrating lymphocyte (TIL) therapy. The goal was to utilize a patient’s own immune cells to fight against cancer. “I read the description and I just knew this was it. This was what I was going to do,” said Melinda. After consulting with her oncologist, Melinda and her family began the process of applying for the trial on their own.They filled out the forms, sent in the scans, and even sent in blood samples themselves. Despite a number of hurdles in her path, Melinda advocated for herself and was accepted into the trial. While the eight patients treated before her on the trial had failed to respond to treatment, Melinda remained hopeful. “I was just excited to finally have an option,” she said. Entering the trial, Melinda Bachini became known as patient 3737.
C.jpg)
The method that Dr. Rosenberg and his team were testing involved surgically removing a portion of the tumor, separating out the immune cells that had infiltrated the tumor, encouraging those cells to multiply in a laboratory, and delivering the cells back to the patient as a drug. The researchers also analyzed the tumor samples for genetic mutations, identifying only 26 mutations in patient 3737 that were likely to raise red flags that the immune system could hunt for. Next, the researchers tested whether any of the immune cells isolated from the tumors were able to specifically recognize tumor cells. They found a population of immune cells, CD4+ T cells, that responded to one particular mutation that distinguished the tumor cells from their healthy counterparts. Hopeful that the expanded immune cells would be able to react against tumors, the researchers delivered a dose of 42 billion T cells into patient 3737’s system (about 25% of which were specific for the mutation) followed by four doses of IL-2 (a naturally occurring signaling molecule of the immune system) to help the transferred T cells to continue multiplying within the body.
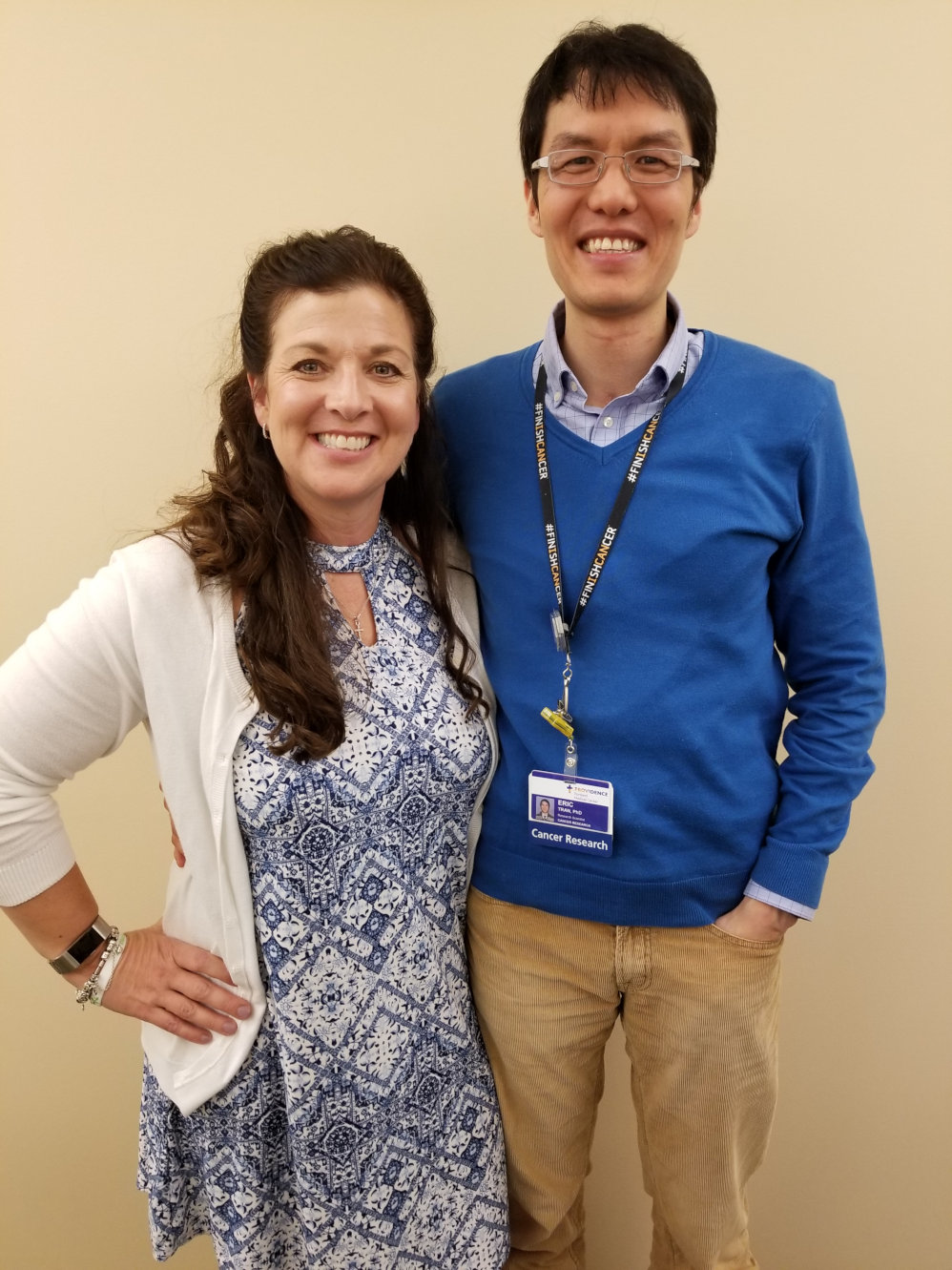
The science behind the study was innovative and complex, but Dr. Tran made sure to keep his patients in the loop. According to Melinda, he always took the time to come out of the lab and explain exactly what was going on. He even took Melinda and her husband into the lab to show what was happening behind the scenes and under the microscope. This transparency gave Melinda comfort and confidence throughout her clinical trial experience.
“Every day got a little bit better. My coughing started to subside. I could laugh. I could walk the dog again.”
After Melinda was treated, a cellular war began in her body, with the transferred cells battling her many tumors. “The initial treatment was tough, but unlike with chemo, I at least knew the discomfort of it wasn’t going to be long-term, and that I just had to get to the other side of it,” she said. Once released from the hospital, Melinda quickly began noticing improvements in her daily life. “Every day got a little bit better. My coughing started to subside. I could laugh. I could walk the dog again,” she said. Going back for her one-month check up, Melinda felt great. Her doctors were cautiously optimistic; they wouldn’t say for sure that the treatment was actually working, but Melinda could feel that it was.

Two months after the initial dose of treatment, the tumors in Melinda’s liver and lungs officially showed evidence of regression, and continued to shrink until seven months post-treatment. Melinda’s disease stabilized, but after seven months of stable disease, the tumors within the lungs, but not the liver, began to grow again. It was a disappointing result, but neither Melinda nor the researchers were ready to give up.
To better understand how the treatment initially worked and why it eventually lost steam, the researchers took more blood and tumor samples and found that many of the mutation-reactive T cells they had used to treat Melinda were still present in her blood and tumors. Many of these cells had even taken on “memory” properties that would allow them to persist in the body and stand guard against future threats. Fortunately, Melinda’s tumors still expressed the targeted mutation. Dr. Rosenberg and Dr. Tran were confident that another more potent dose of T cells would revitalize the antitumor response they had seen initially. Melinda felt good about being treated again, explaining that Dr. Rosenberg’s excitement was contagious.
Melinda’s second dose consisted of 126 billion cells, 95% of which were specific for the mutation. Once again, Melinda responded to the treatment and her tumors began to rapidly shrink. “It worked so fast and so well. My quality of life increased so dramatically. A month later I was downhill skiing!” said Melinda. This response was ongoing when the trial closed. After the trial closed, Melinda’s disease remained stable for two and a half years before she required an additional surgery and treatment with another immunotherapy, PD-1 blockade, which she again responded well to. While she is not officially considered free of disease, 10 years after her initial diagnosis, Melinda is healthy and confident that she will remain so.
The story of patient 3737 was picked up by a number of major news outlets and was widely shared by both scientists and patients alike. Shortly after the stories broke, Melinda chose to shed the anonymity of her patient number, instead recognizing the important role she could play as a patient advocate. “I don’t want my story to give anyone false hope because there is no guarantee with clinical trials, or with this treatment in particular,” said Melinda. “To me the important thing is to remind patients that there is information out there, and that there is research being done.”
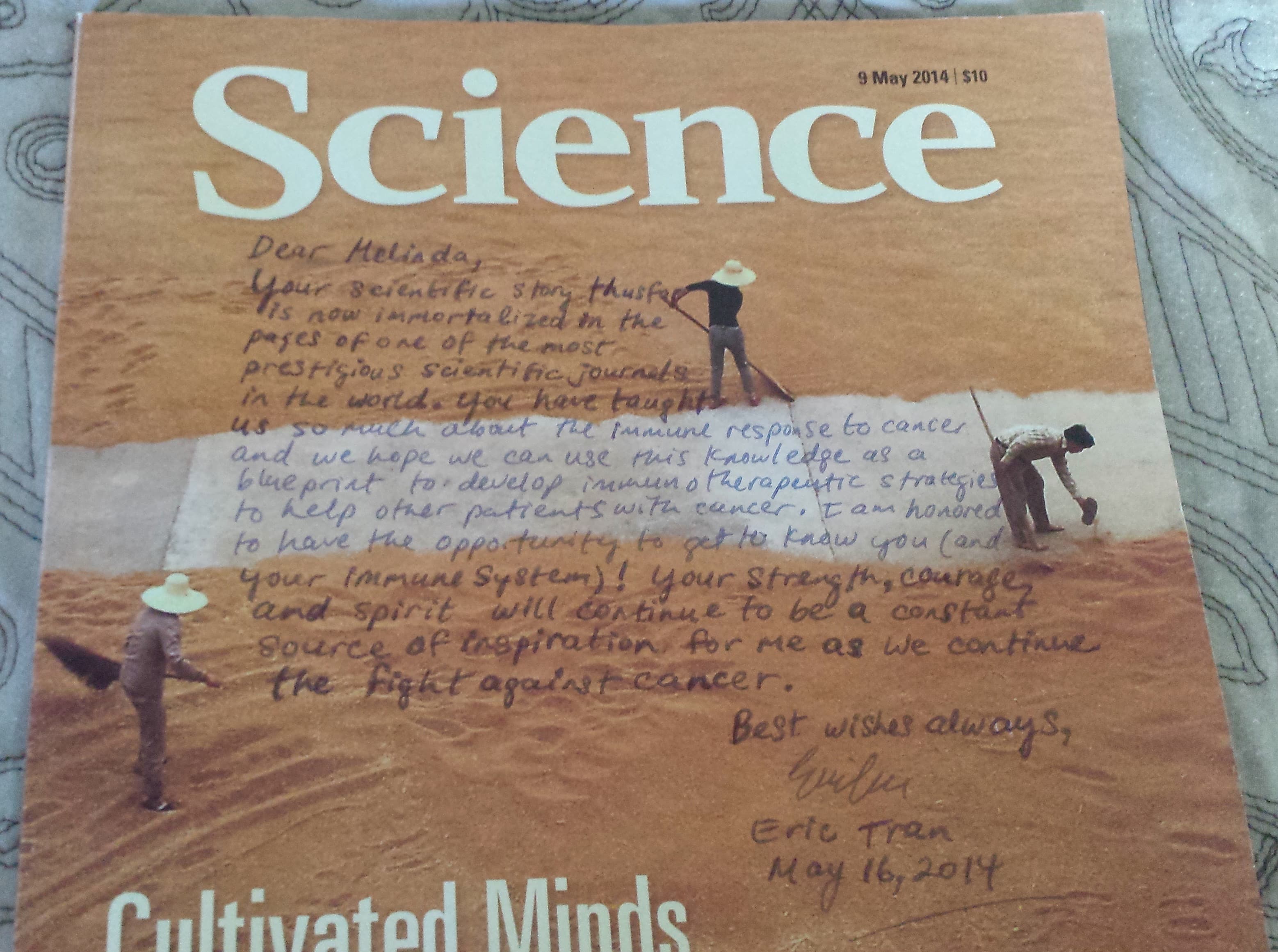
When the original case study by Dr. Rosenberg and Dr. Tran appeared in the journal Science in 2014, Dr. Tran sent Melinda a copy of the issue, personalized with a note:
“Dear Melinda,
Your scientific story thus far is now immortalized in the pages of one of the most prestigious scientific journals in the world. You have taught us so much about the immune response to cancer and we hope we can use this knowledge as a blueprint to develop immunotherapeutic strategies to help other patients with cancer. I am honored to have the opportunity to get to know you (and your immune system)! Your strength, courage, and spirit will continue to be a constant source of inspiration for me as we continue the fight against cancer.
Best wishes always, Eric Tran”
Meet the researcher:
The groundbreaking study was led by Eric Tran, PhD, who at this time was a research fellow with Steven Rosenberg, MD, PhD at the National Cancer Institute, National Institutes of Health. We spoke with Dr. Tran:
How and why did you get involved in this clinical study?
Since university, my lifelong goal has been to harness the immune response to fight cancer. I was fortunate to be mentored by Dr. Steve Rosenberg as a postdoctoral fellow at the NCI where I was given an opportunity to develop more effective immunotherapies for patients with cancer. At the time, we wanted to test whether we could cause tumors to shrink and go away by harnessing T cells that targeted mutations (neoantigens) expressed by the patient’s own cancer. Melinda was the first patient on our clinical trial where we found neoantigen-reactive T cells and were able to harness them for therapy.
How did you feel seeing the outstanding clinical response in Melinda Bachini?
When we first saw evidence of tumor shrinkage at her first follow-up visit (after her second T cell infusion), I felt some relief and cautious optimism, but at the same time I knew all too well that this could be a short-term response and that only time would tell how effective the therapy would be. Melinda’s tumor regression occurred over a period of several years, so I relived the cycle of anxiousness, relief, and cautious optimism over and over again! But I am absolutely ecstatic for Melinda that she continues to do well.
How have the results observed in Melinda shaped research in this field? How can her success be extended to more patients in the future?
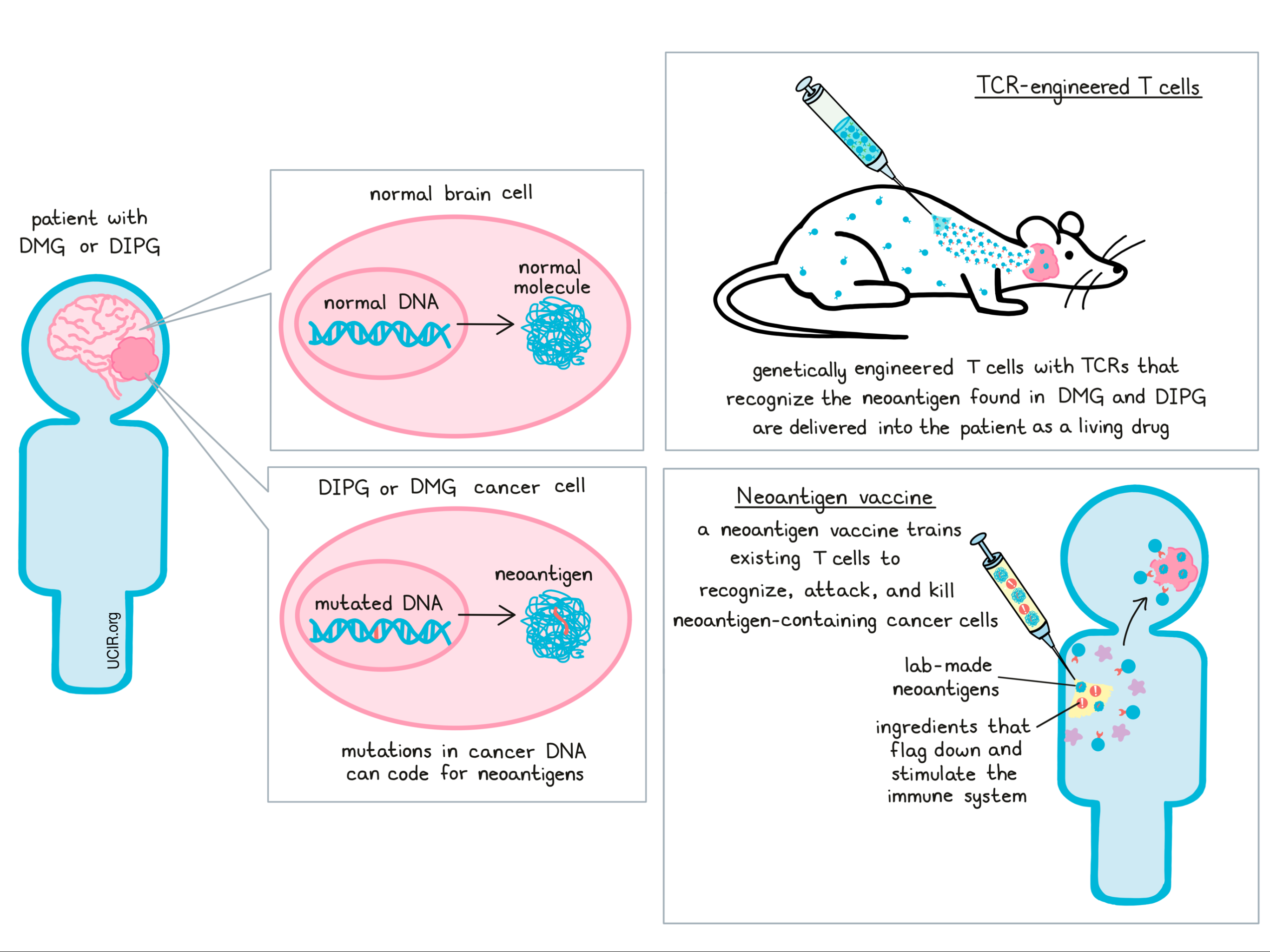
Melinda’s case was the first demonstration that T cells targeting a tumor mutation could mediate the regression of metastatic epithelial cancer. Thus, her story provided evidence that harnessing T cells that target unique mutations expressed by the patient’s own cancer may be a feasible and effective strategy that could be applied to other patients with cancer. Indeed, her success has already catalyzed the exploration and development of novel and highly personalized cancer immunotherapies targeting neoantigens, as witnessed by the recent surge in the number of research groups and companies worldwide that are now developing neoantigen-targeted vaccines or adoptive T cell therapies. Although these efforts hold great promise, not all patients have, or will experience clinical responses after treatment with therapies that target neoantigens. We must better understand the mechanisms behind why these patients don’t experience clinical responses so that we can develop the next generation of more effective cancer immunotherapies.
by Lauren Hitchings
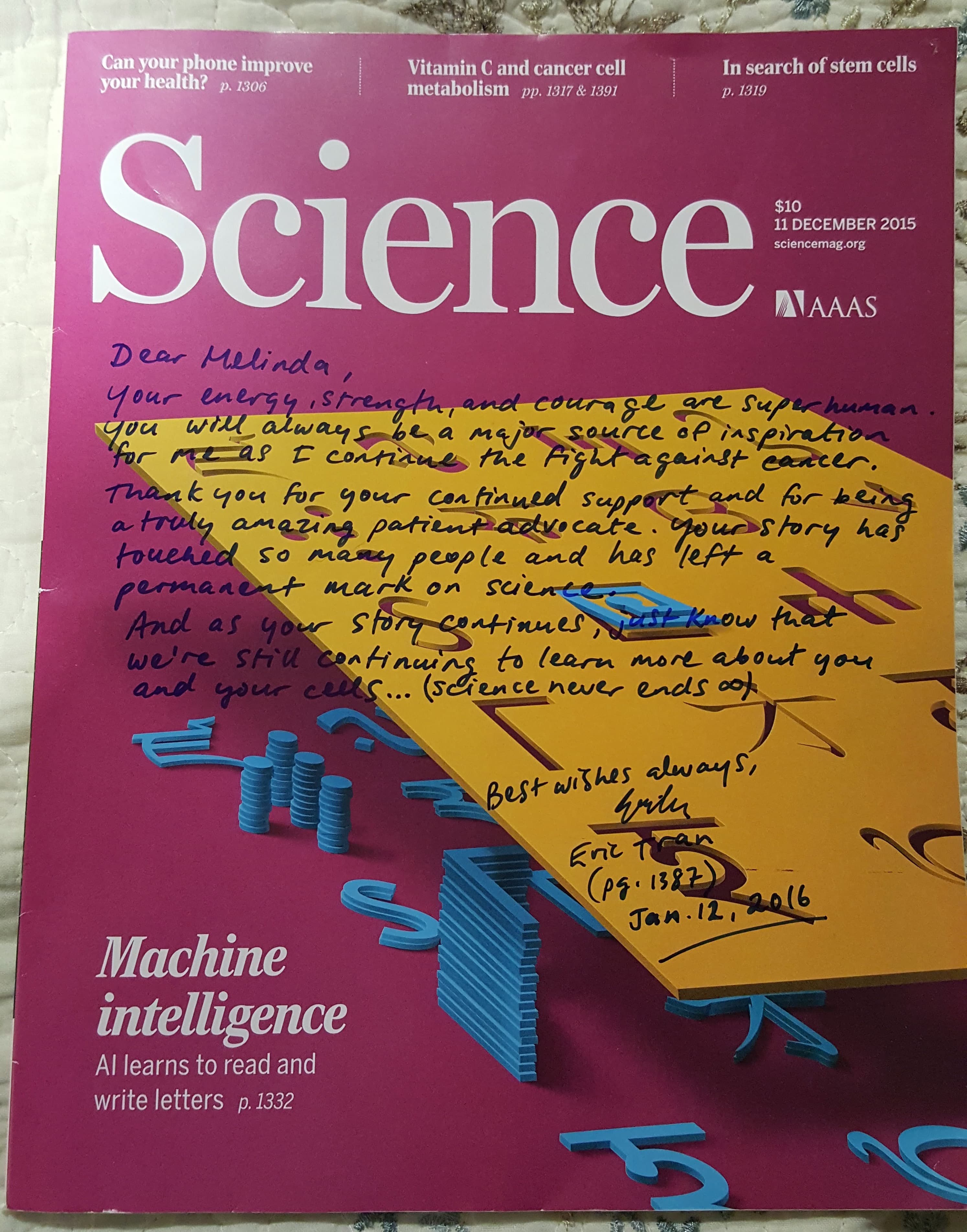
“Dear Melinda,
Your energy, strength, and courage are superhuman. You will always be a major source of inspiration for me as I continue the fight against cancer. Thank you for your continued support and for being a truly amazing patient advocate. Your story has touched so many people and has left a permanent mark on science. And as your story continues, just know that we’re still continuing to learn more about you and your cells… (science never ends ∞) Best wishes always, Eric Tran- Jan. 12 2016”
References:
N/A