Cancer Vaccines
What are vaccines?
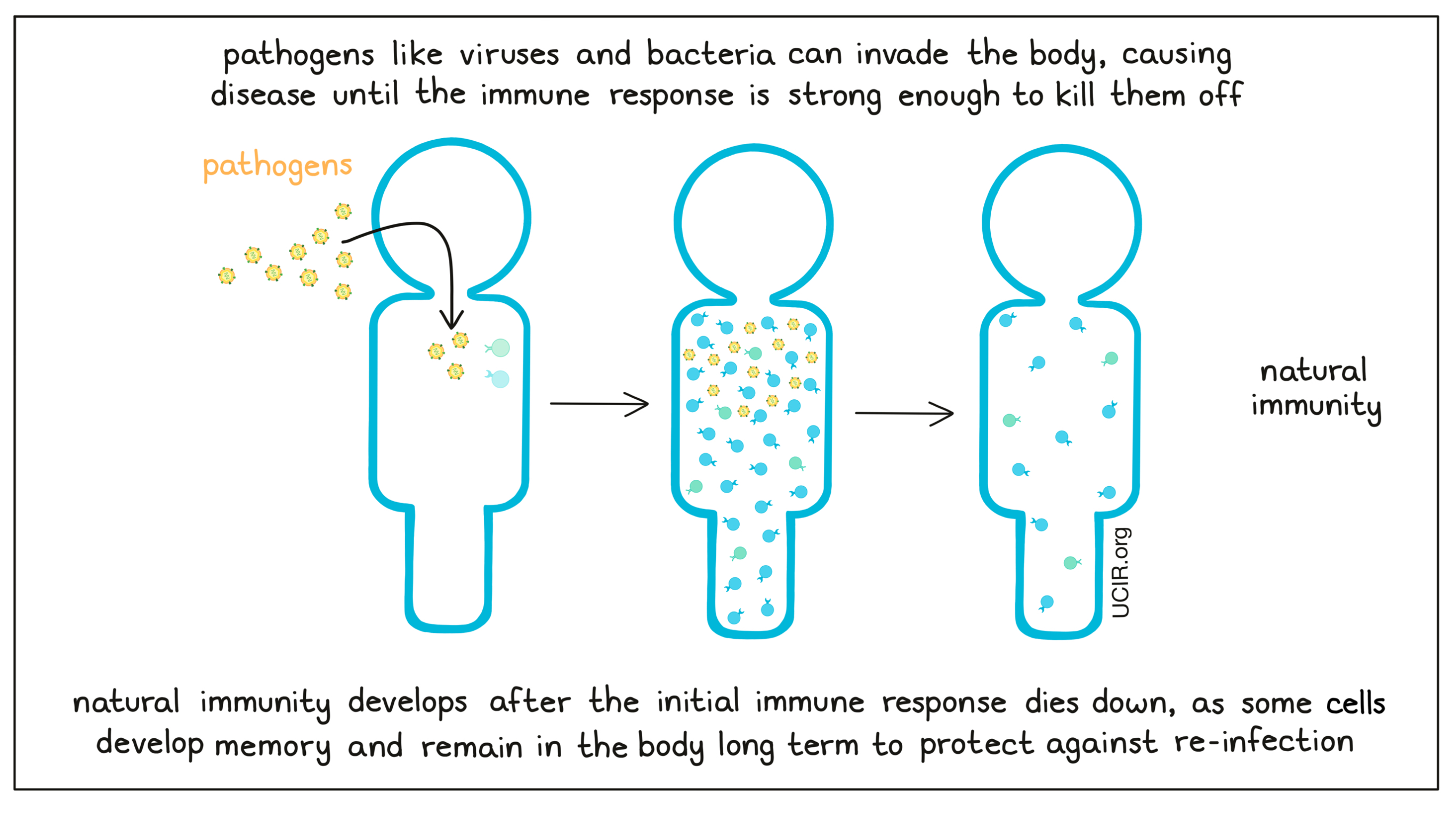
A vaccine is a type of immunotherapy that can be administered to protect the recipient against one or more diseases. Vaccines to prevent the spread of serious and even life-threatening infectious diseases, such as smallpox, polio, and diphtheria, have had a profound positive effect on global health. The concept of vaccination was discovered when people observed that individuals who recovered from some infectious diseases developed “natural immunity” or resistance to reinfection with the same disease.
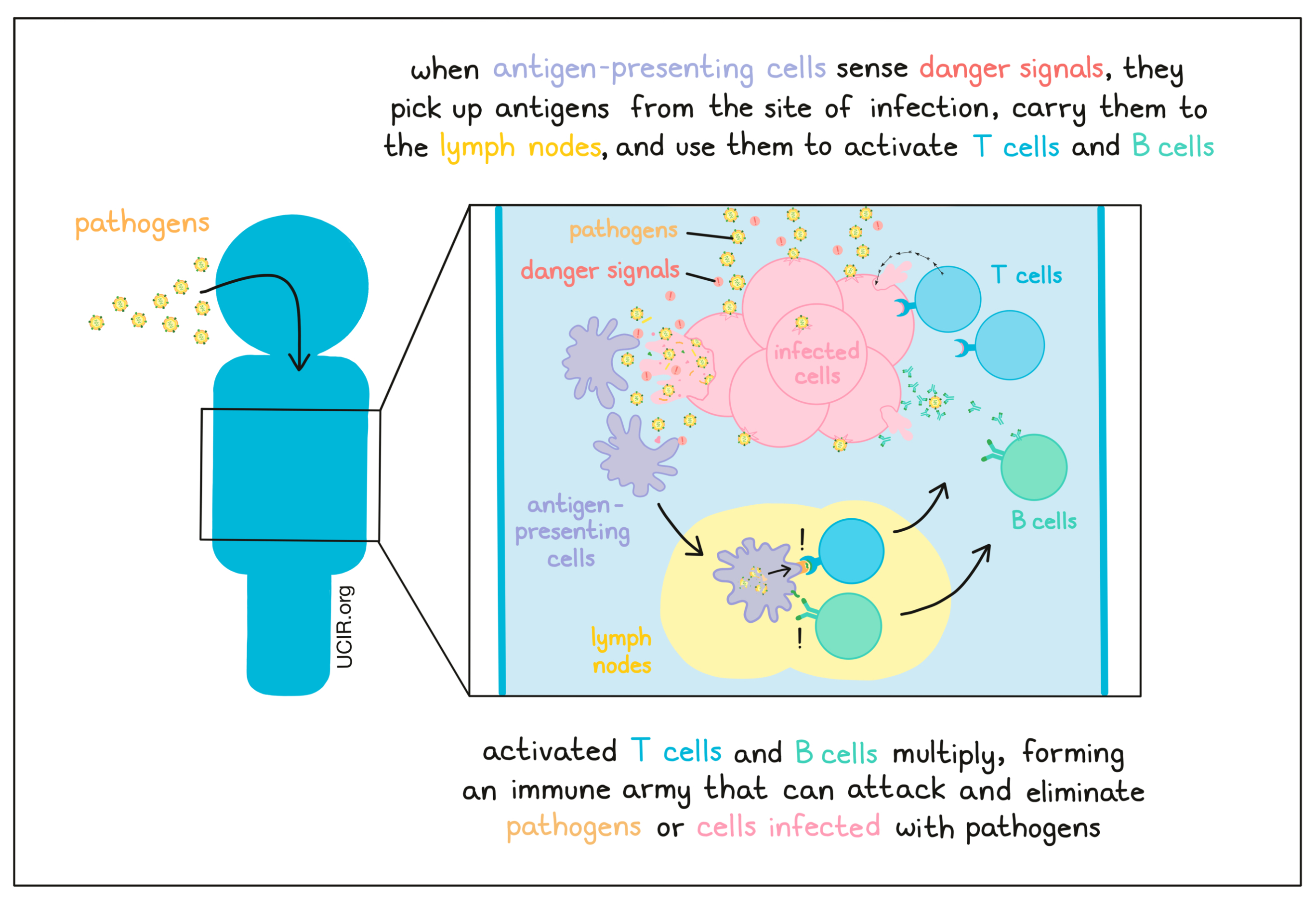
When the body is exposed to a “pathogen” (like a virus or bacteria), the immune system is able to recognize it as foreign or “non-self” based on the presence of antigens – protein molecules that are not typically found in a normal, healthy body. Pathogenic infections also tend to damage cells in the body, leaving a trail of “danger signals” – molecules released by pathogens or infected cells, or patterns of damage that alert patrolling immune cells that something is not right in the body. Once the immune system detects a threat, a multitude of immune cells move in to launch a coordinated attack. Some cells attack immediately on site, while others need to be called to the scene. This occurs when antigen-presenting cells, the most potent of which are called dendritic cells, pick up debris, including antigens, from the site of the infection and carry them to the lymph nodes, where they present the antigens to B cells, and T cells. B cells (which release antibodies) and T cells (the warriors of the immune system) can then multiply, forming an immune army that can launch a secondary immune attack that is stronger and more targeted towards the particular pathogen, or towards cells infected with that pathogen.
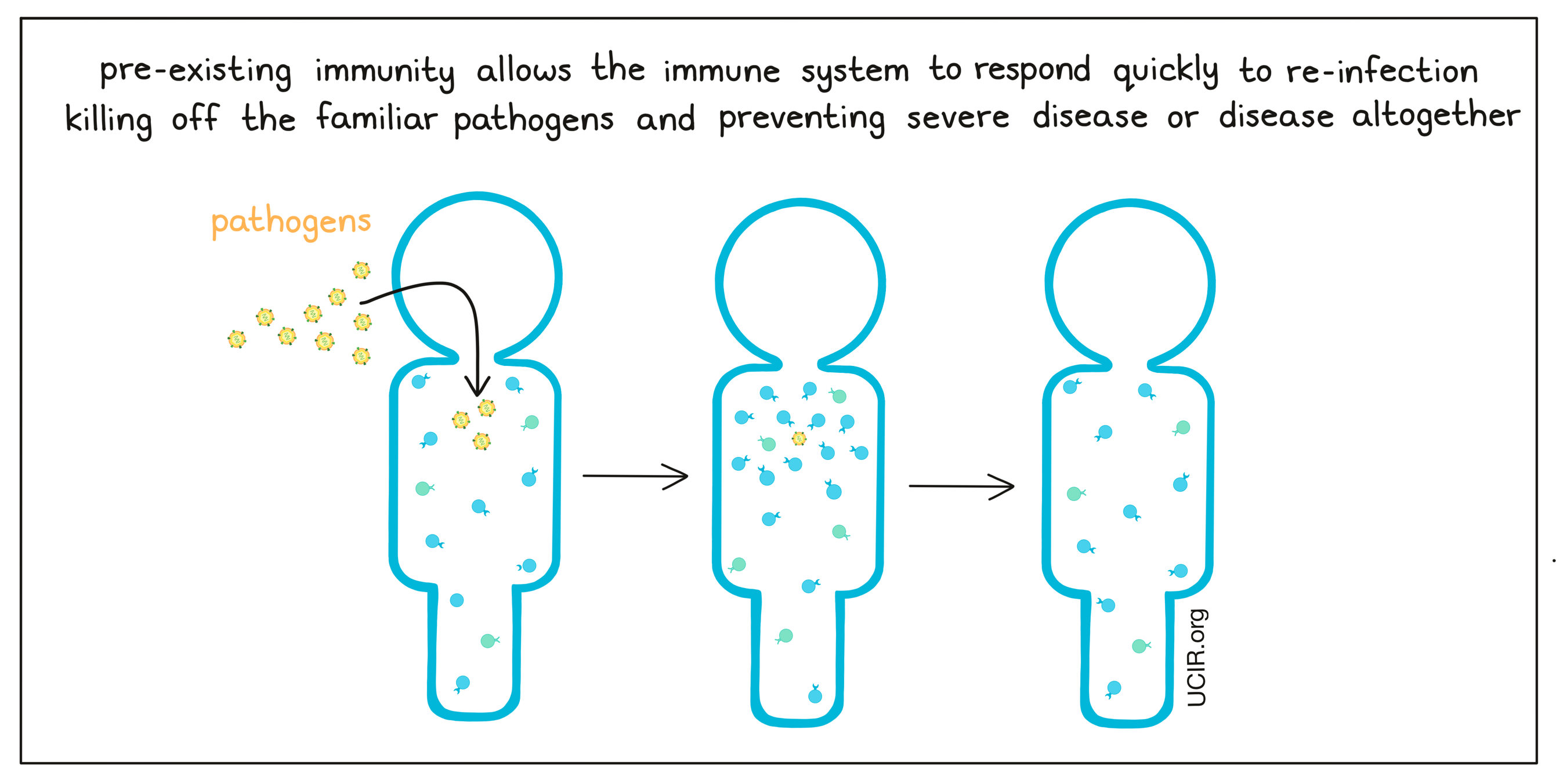
Once a pathogen has been eliminated from the body, the immune response begins to die down. While most of the T and B cells die off, some develop memory and remain in the body long term, ready to attack the same threat should it appear again.
Vaccines are used as a way to to safely stimulate immune responses and long-term immune memory against specific threats in the same way that a natural infection would. They mimic naturally occurring pathogens and work by introducing the body to the potential threat without actually introducing an active version of the threat, allowing the body to build immunity without risking the damage that a real infection would cause.
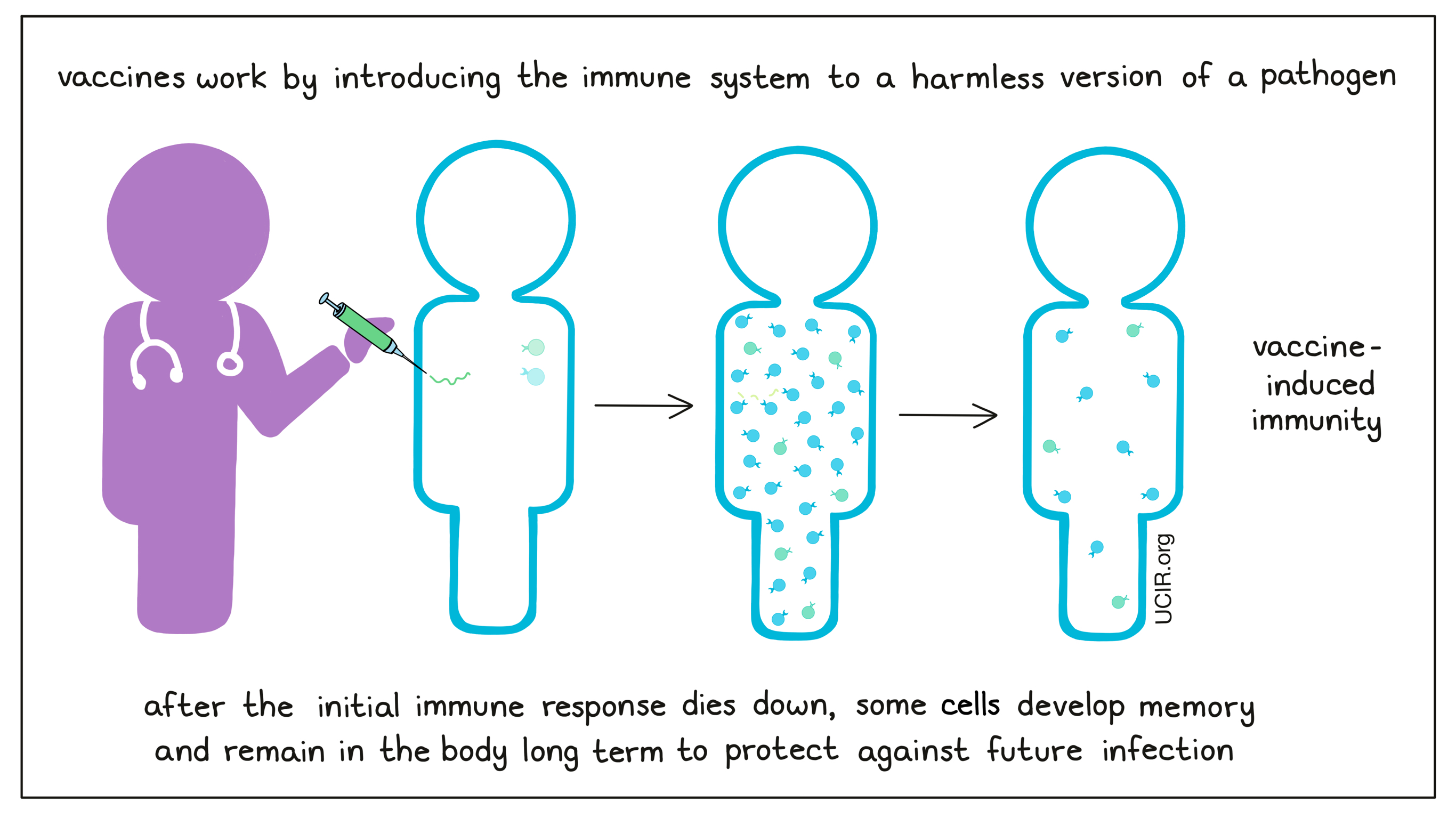
If a person has pre-existing immunity to a specific threat, whether it was induced by prior infection or by vaccination, the body is prepared against future infection. If the same pathogen enters the body, the immune system stands armed and ready to launch a quick, strong response to eliminate the pathogen, preventing severe disease, or disease altogether.
Vaccines to protect against pathogens
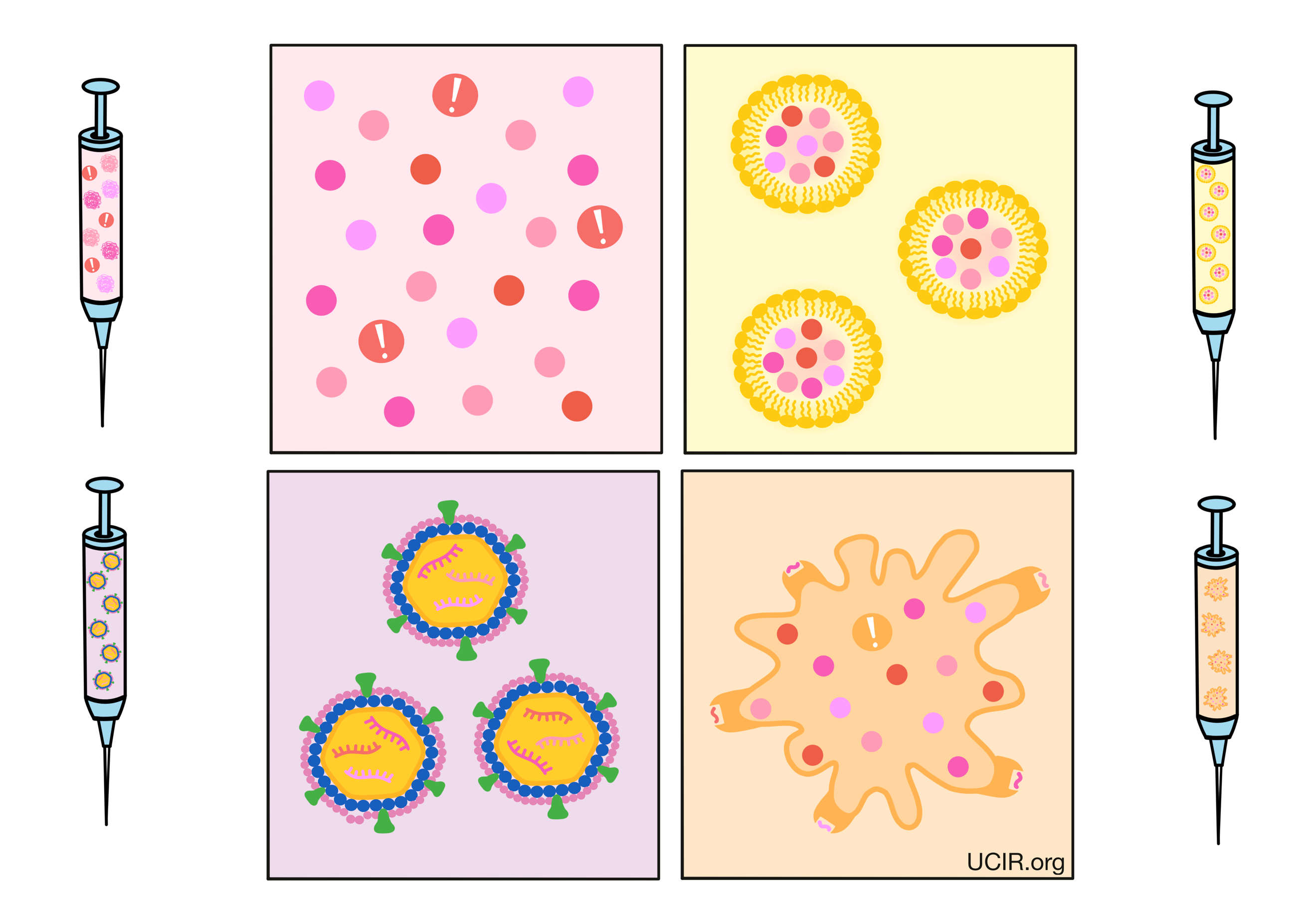
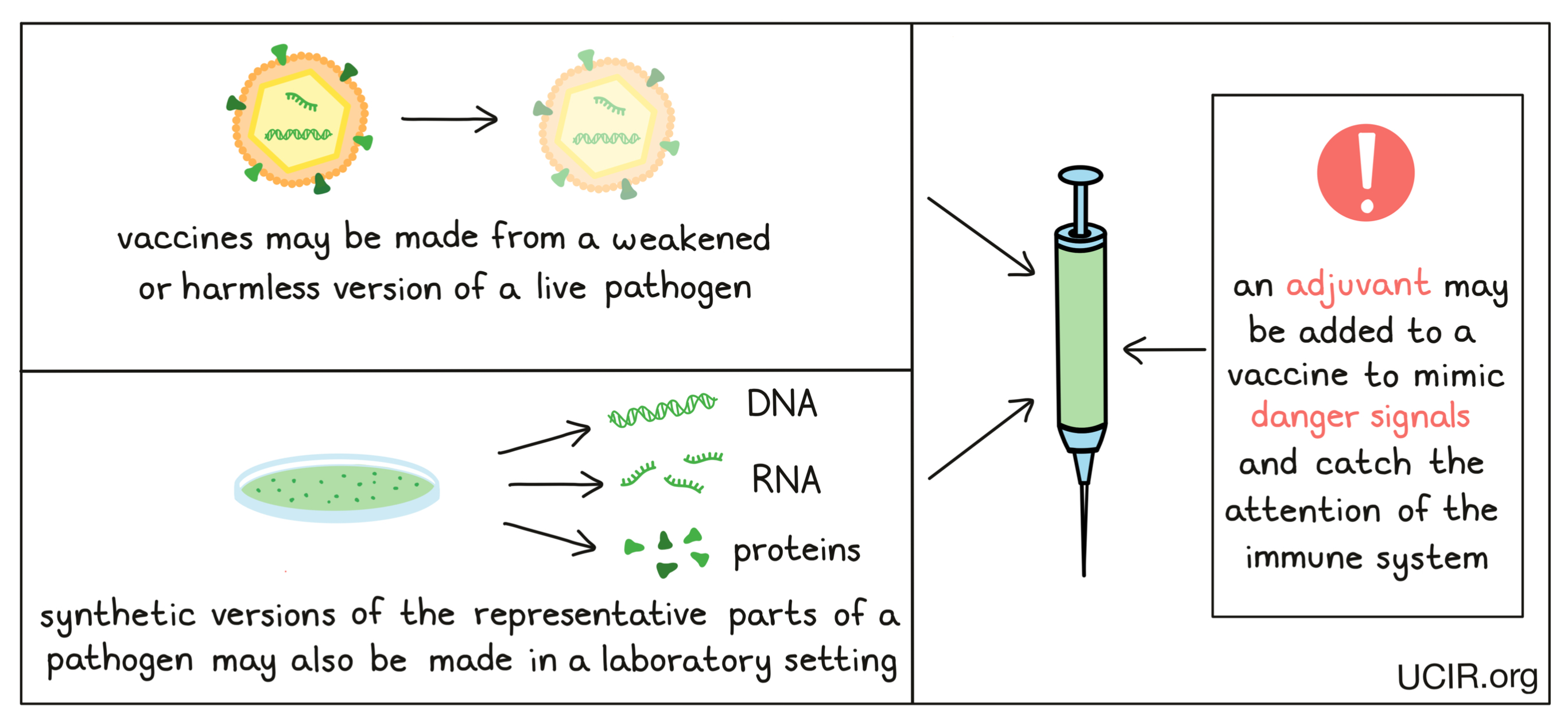
Vaccines can be created in a variety of different ways. Some may incorporate weakened/harmless forms of the live pathogen, so that symptoms are mild, but immunity still develops. Other vaccines may only contain antigens from the pathogen (e.g., particular proteins, or DNA or RNA coding for proteins that are unique to a pathogen and can be recognized by the immune system). The antigens in vaccines are generally synthetic versions of proteins that have been generated in a laboratory. Vaccines may also include an adjuvant – an additional ingredient that catches the attention of the immune system and mimics danger signals, ensuring that the immune system takes notice of the vaccine antigens and responds to them as if they were a real threat.
Vaccines to treat cancer
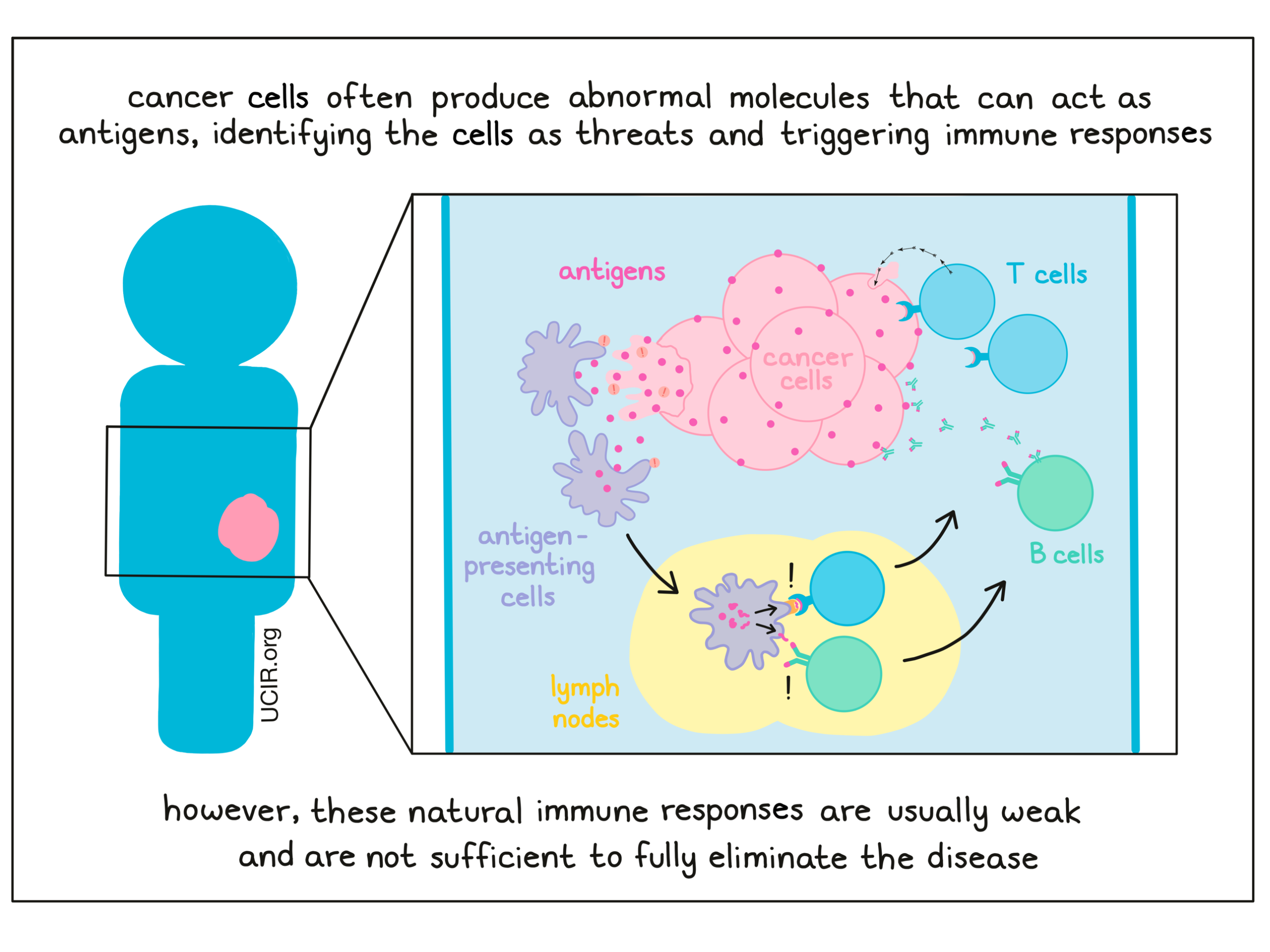
While vaccines have typically been used to prevent diseases, they can also be used as treatments for existing diseases by encouraging the immune system to respond more strongly against a particular threat. Vaccines used as treatments for existing diseases are called therapeutic vaccines. Cancer is a disease caused by mutations in the DNA of a cell that cause it to change and multiply out of control. These changes may include the production of abnormal molecules, which can act as antigens and make the cancer cells look different from healthy cells – like a threat. Research has shown that patients often develop an immune response to their cancer, but one that is typically inadequate to cure them of the disease. This may be because, unlike pathogens, cancer cells closely resemble healthy cells, and so they may not always catch the attention of the immune system. Cancer cells also often develop ways to evade the immune system or defend themselves against immune attacks. If the immune system fails to catch and kill cancer cells early on, the cancer will continue to grow in the body, causing disease.
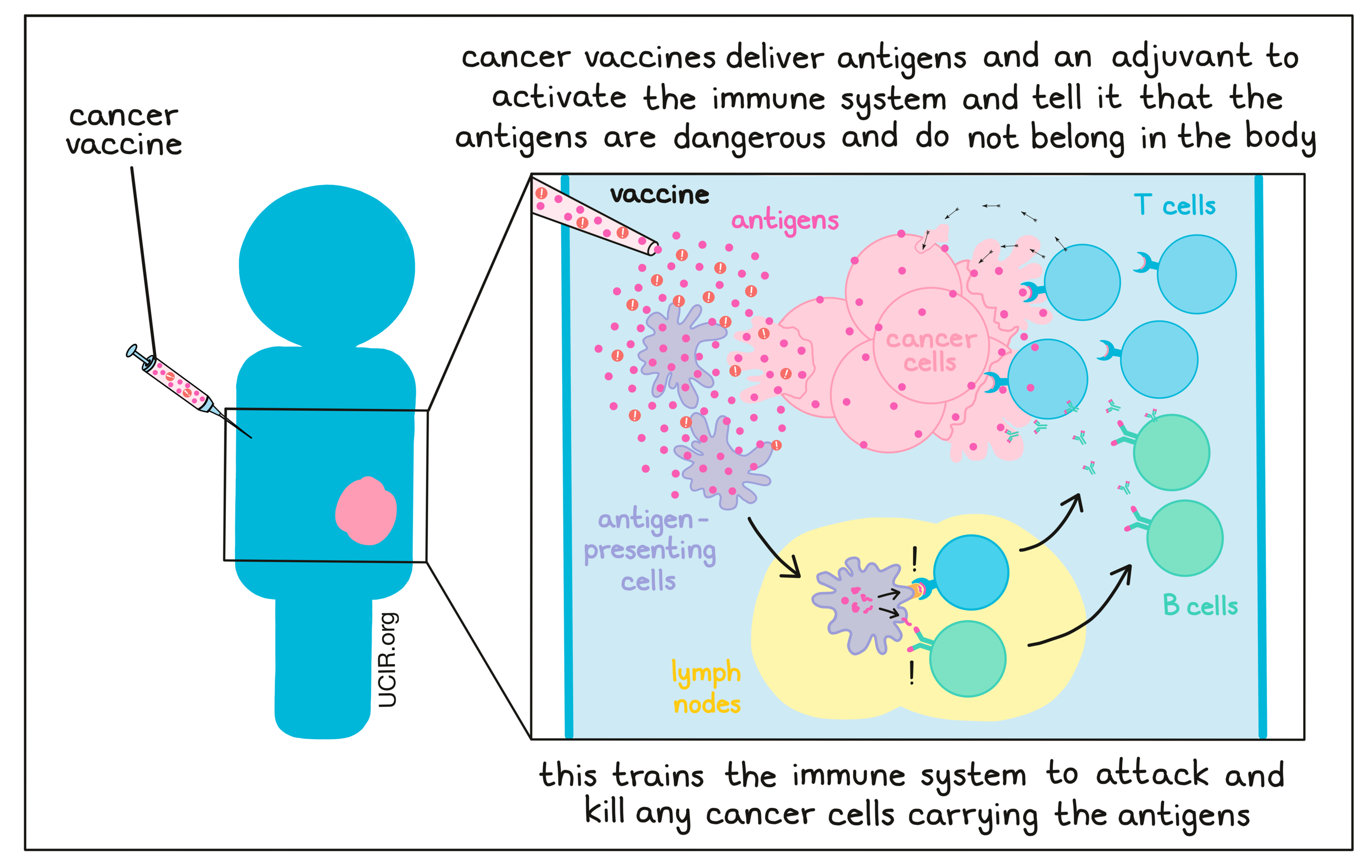
In recent years, researchers have developed numerous strategies to both enhance existing immune responses and trigger new immune responses to cancer. With cancer vaccination, the idea is to introduce the immune system to cancer in a way that trains it to strongly recognize the cancer as the threat that it is. This drives immune cells to attack the cancer as foreign, eliminate it from the body, and protect the patient long-term from re-emergence of disease (cancer recurrence or relapse).
How do cancer vaccines work?
Like vaccines that protect against pathogens, vaccines that treat cancer work by introducing cancer to the immune system in a way that triggers a strong immune response. Developing a cancer vaccine is usually a personalized process that involves identifying and selecting antigens that are unique to a patient’s cancer (i.e., not found in normal, healthy cells in the body) and can be recognized by the immune system. Once selected, these antigens can be included in a vaccine. Currently there are many different strategies for both choosing antigens and delivering vaccines.
What are the different types of antigens used for cancer vaccines?
Effective vaccination depends first and foremost on which antigens are incorporated into the vaccine. Choosing which antigen or antigens to target is one of the biggest challenges in the development of cancer vaccines. Generally, strong target antigens should be unique to the cancer (so that the immune system does not attack any healthy cells) and readily recognized by the immune system. The types of antigens that have been used in cancer vaccines fall into three categories:
1- Cancer-associated antigens
Cancer-associated antigens (sometimes called tumor-associated antigens) are antigens that arise when changes in cancer cells cause them to behave abnormally and to produce proteins inappropriately. For example, cancer cells may produce excess amounts of a particular protein, produce a protein in the wrong cell or tissue type (e.g., cancer testis antigens – proteins typically only produced in the testes or placenta), or produce a protein at the wrong time (e.g., germline antigens – proteins that are usually only produced during prenatal development or in germ cells [sperm and egg]).
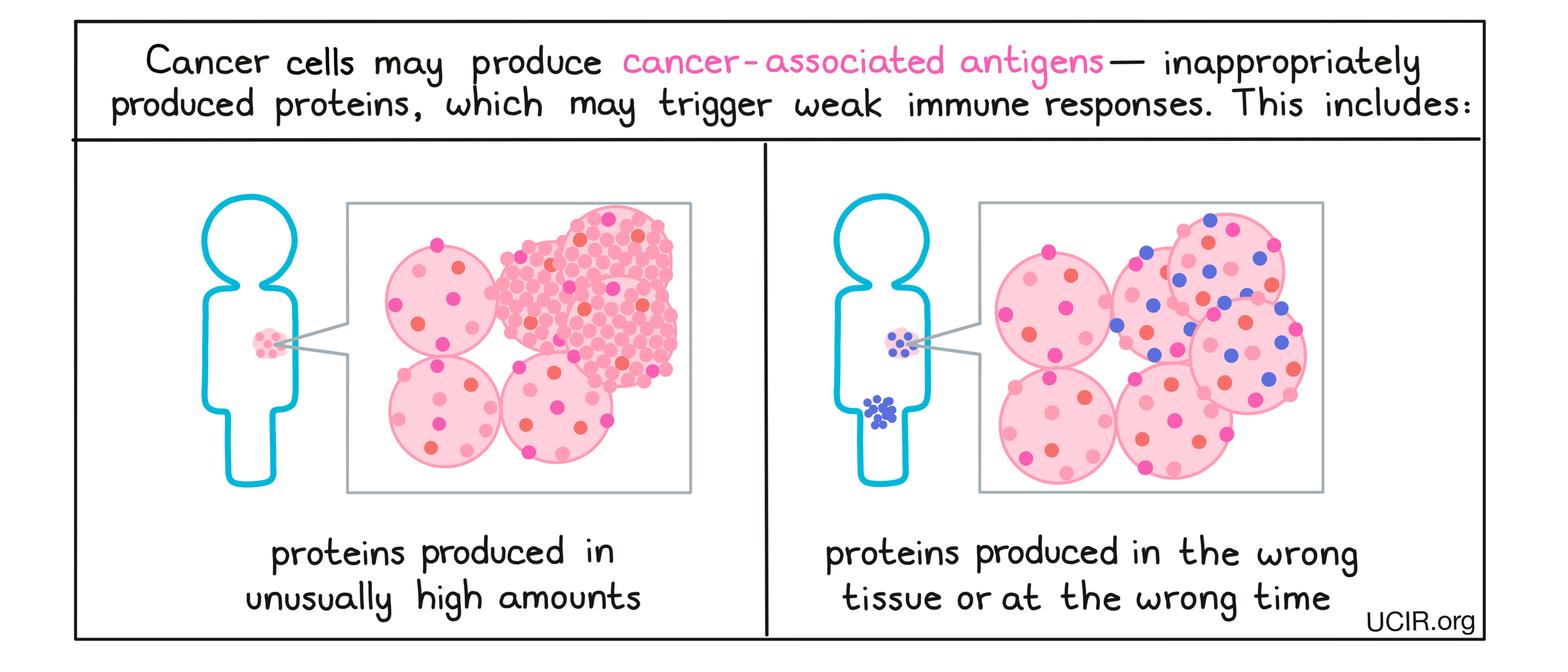
These out-of-place proteins may be recognized by the immune system as inappropriate or “non-self”, though the natural immune responses to cancer-associated antigens is often weak, as these types of antigens are not entirely foreign to the body. However, vaccines can be used to initiate or enhance responses against them. For a cancer-associated antigen to make a good vaccine target, it must be recognized by the immune system and be absent or nearly absent in normal tissue, present only in normal tissues that are not essential for health, or present only in tissues that cannot be accessed by immune cells. This ensures that when the vaccine is given, the immune response only damages and kills cancer cells, and not healthy cells in the body.
While most cancer-associated antigens are unique to a patient, some are frequently present in certain cancer types. For this cancer-associated antigens, vaccines can potentially be prepared ahead of time, allowing for fast and cost-effective treatment. However, patients would still have to be tested before treatment to be sure that the cancer-associated antigen is present and at high levels in their particular case.
2- Neoantigens
Neoantigens are antigens that arise when a mutation in the DNA of cancer cells causes them to produce a mutated protein that is entirely new to the body and looks unfamiliar to the immune system. Unlike cancer-associated antigens, these proteins are not produced in any normal, healthy cells in the body, so they stand out to the immune system as “non-self”.
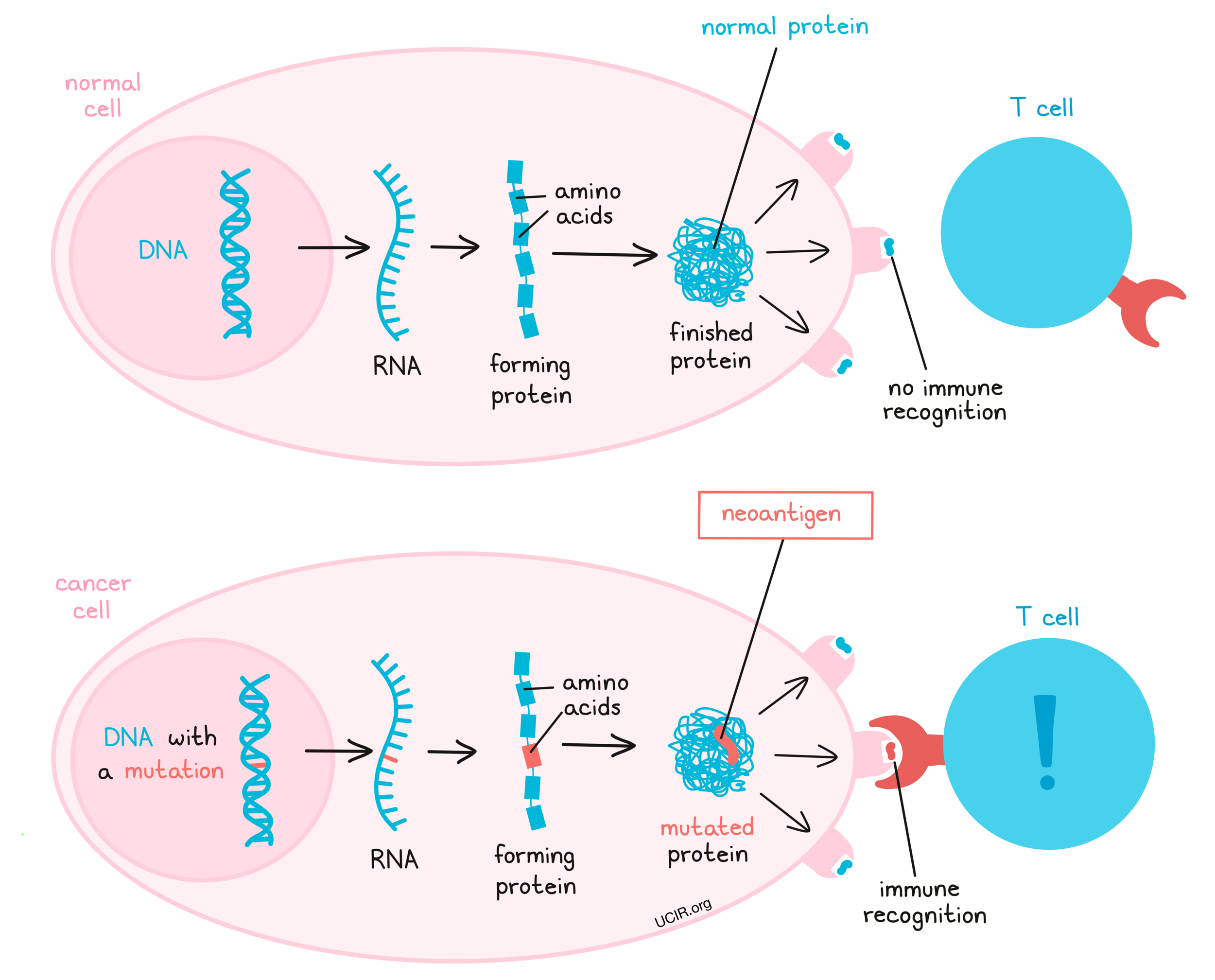
Cancers often develop a large number of mutations, creating many potential neoantigens, and increasing the likelihood that some will be good targets for vaccination. Neoantigen-targeting vaccines can be used to drive a patient’s immune system towards developing a strong immune response that is able to destroy the cancer and prevent the cancer from coming back. Further, the fact that neoantigens are unique to the cancer and are not present in any other tissues means that targeting them is unlikely to harm other tissues in the body. For these reasons, neoantigen vaccines are a major focus for cancer vaccine development.
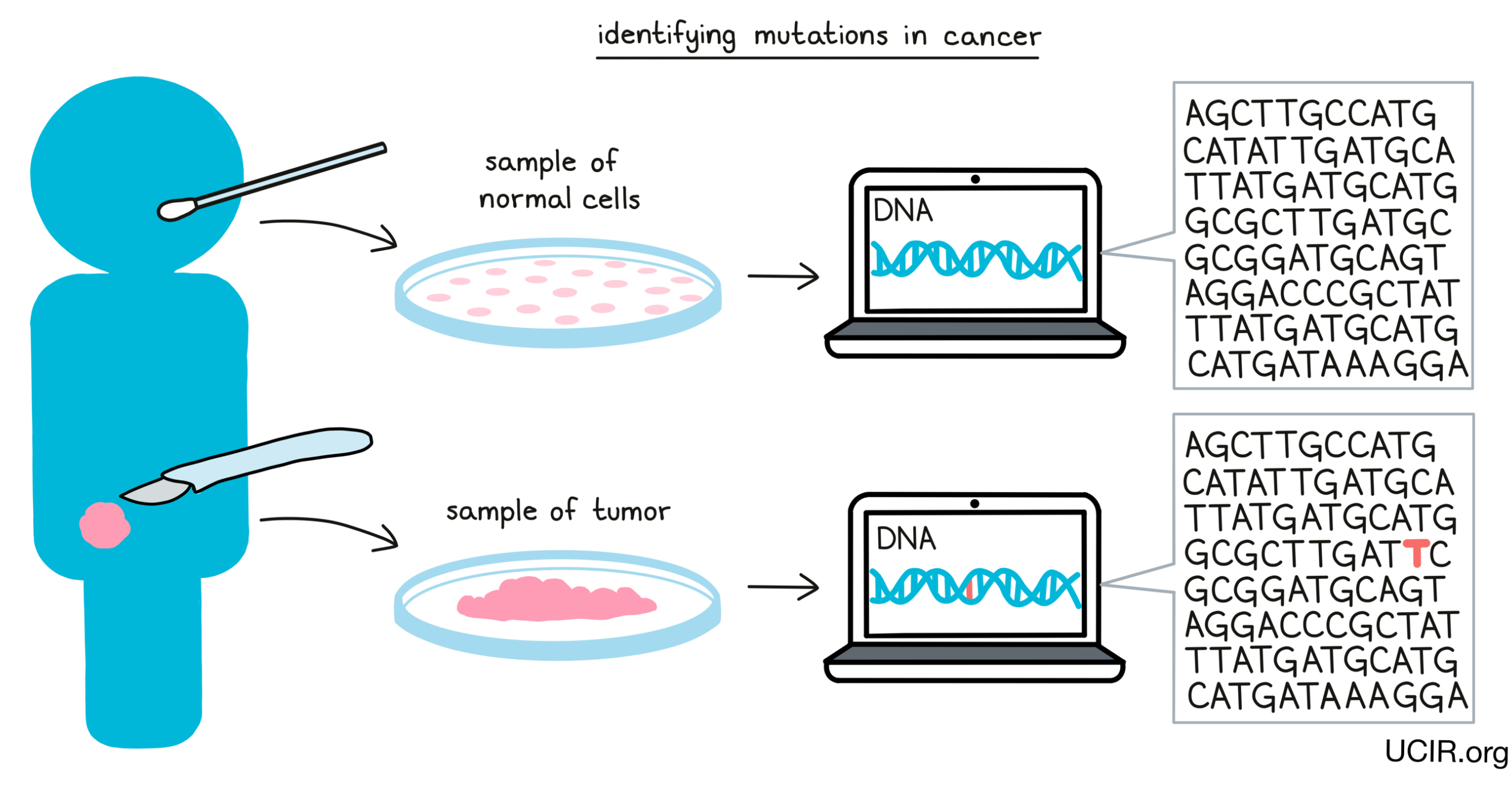
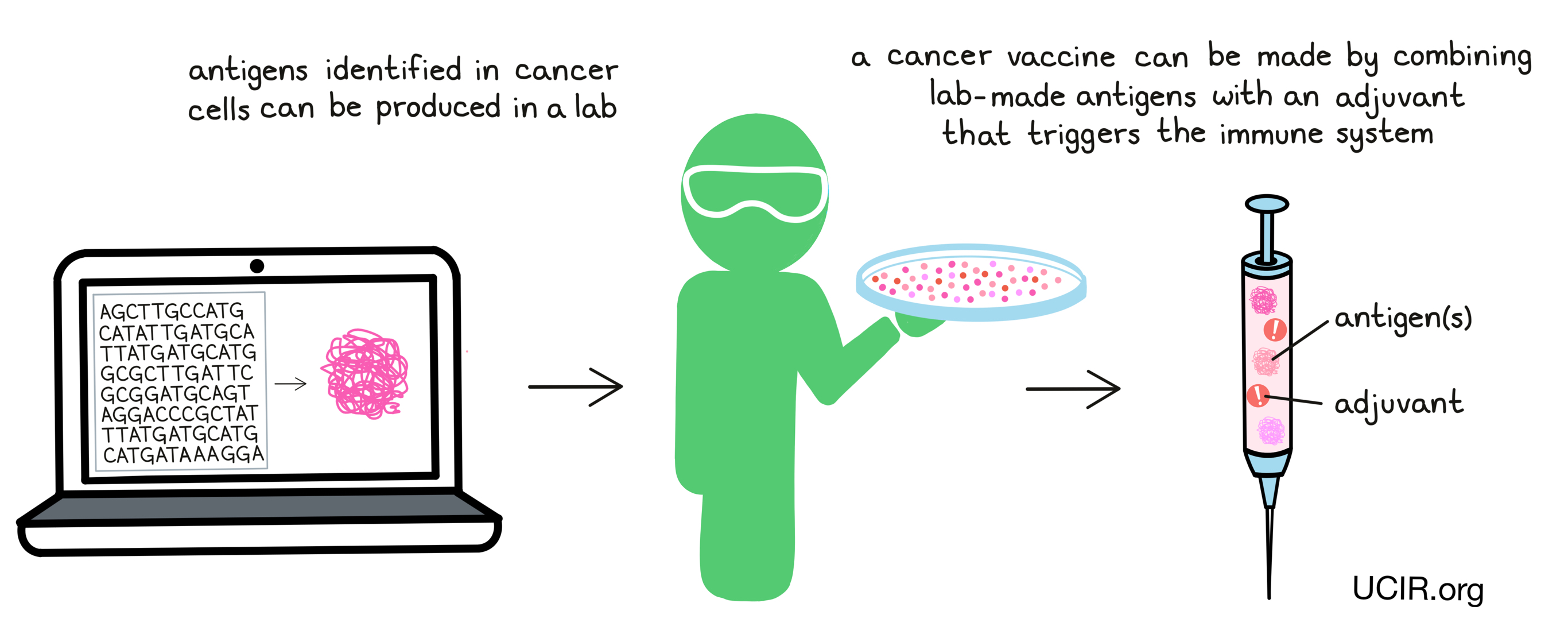
Despite the potential of neoantigen vaccines, there are many challenges in developing them, the first being that almost all neoantigens are unique to each individual and cancer, meaning that neoantigen vaccines must be personalized. To develop a personalized vaccine, researchers must be able to take a sample of the cancer, study the DNA code from cancer cells, compare it against the DNA code in healthy tissue from the individual, identify mutations (changes in the DNA code in cancer vs. healthy cells), analyze whether the mutations actually lead to the production of neoantigens, predict which neoantigens are the most likely to be recognized by the immune system, and decide which neoantigens to include in the production of a vaccine. Then, they must make the neoantigen vaccine product under strict pharmaceutical conditions before giving it to the patient.
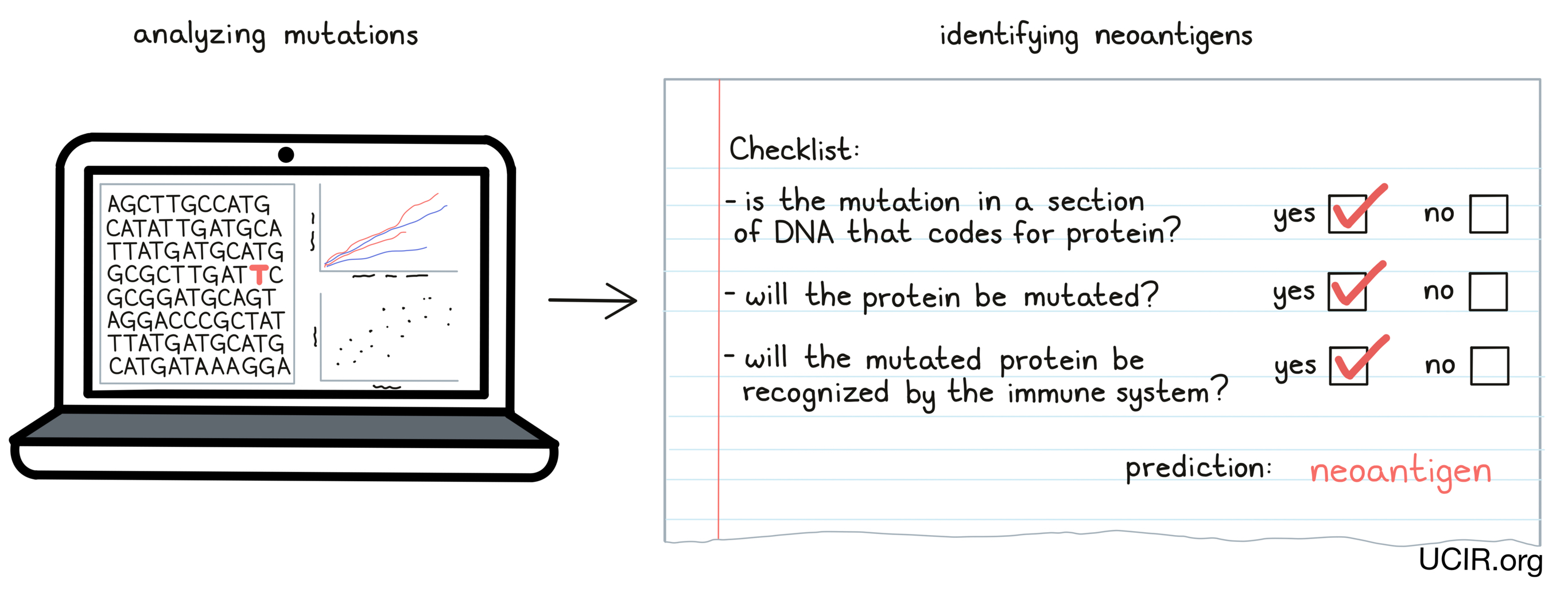
Currently, developing personalized neoantigen vaccines is time-consuming and costly, but methods and technology are improving rapidly, allowing for more efficient production of personalized vaccines. While there are still many hurdles to overcome, targeting neoantigens is considered by many to be the most effective approach to cancer vaccination (see also Neoantigen-based Therapy).
3- Undefined antigens - the whole cancer cell
If a tumor, or part of a tumor can be removed by surgery, it is possible to make a vaccine that includes all of the antigens in the tumor by using samples of the tumor itself. This involves incorporating cancer cells that have been inactivated, killed, and/or broken-up (lysated) into the vaccine. Using this approach, the vaccine would contain nearly every cancer antigen, thus promoting a broad immune response against a variety of antigens. Further, it would help to target all of the cancer cells, as cancer cells may vary, and not all cancer cells contain every antigen.
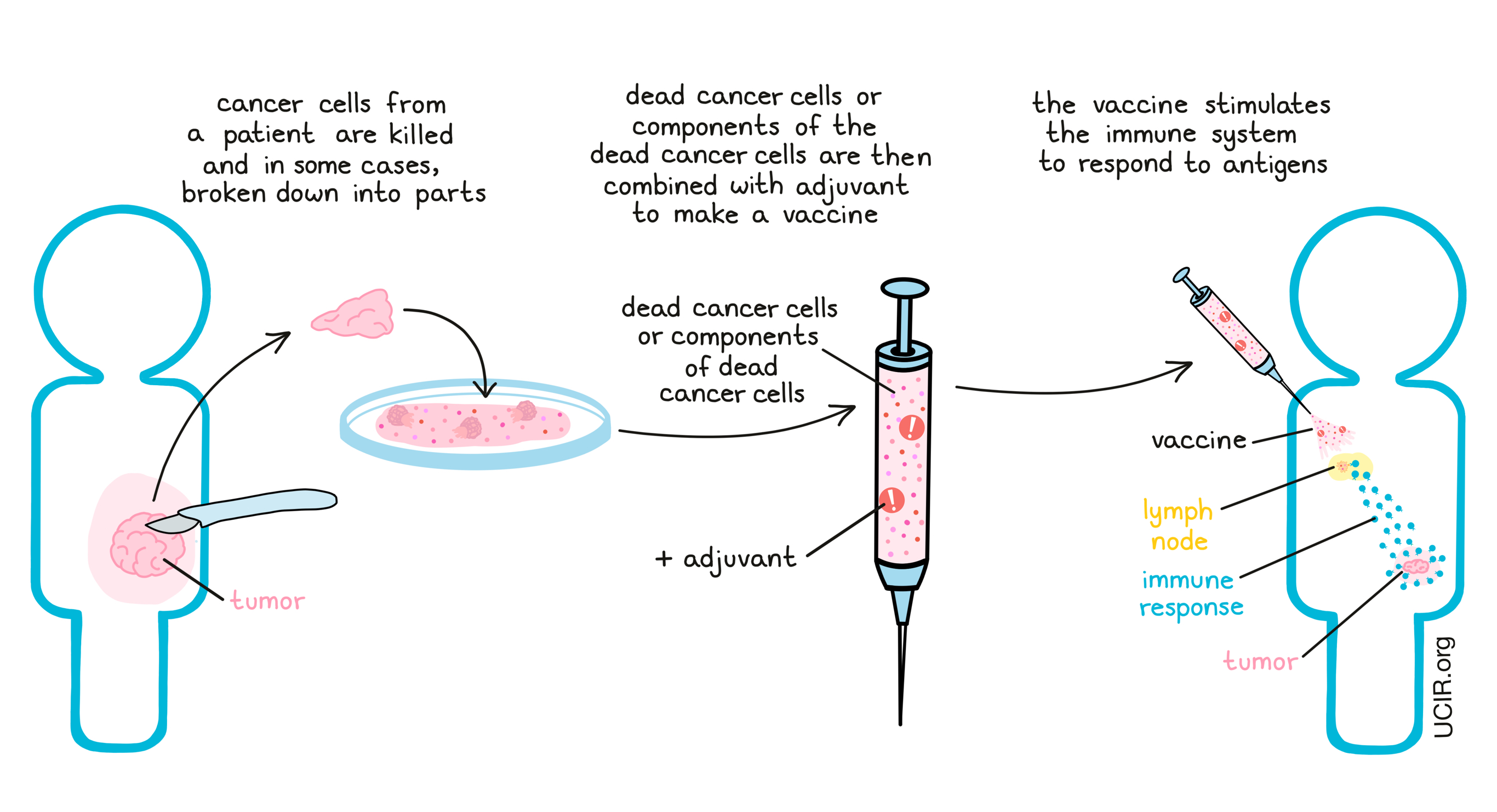
One disadvantage of this approach is that cancer cells also contain many “self” antigens, which are shared with healthy cells. Thus, a vaccine targeting these antigens might promote immune responses that could damage healthy tissues.
A whole cancer cell vaccine or cancer cell lysate works best when it is personalized, meaning that it is prepared from the tumor of the patient. However, this strategy requires a tumor sample, takes time, and can be costly. One alternative to this is to manufacture vaccines from cancer cells of different patients with the same type of cancer. In this case, the vaccine could be prepared ahead of time in large quantities, and could be available as an “off-the-shelf” vaccine – a big benefit. The downside of this type of vaccine is that it would only be useful if it contained antigens that are shared between patients.
How are cancer vaccines made and given to a patient?
Once the desired antigens are identified and chosen, two related questions become critical:
- How will the antigen be made?
- How will the vaccine be delivered?
Making the vaccine: Protein, peptide, DNA, or RNA-based antigens
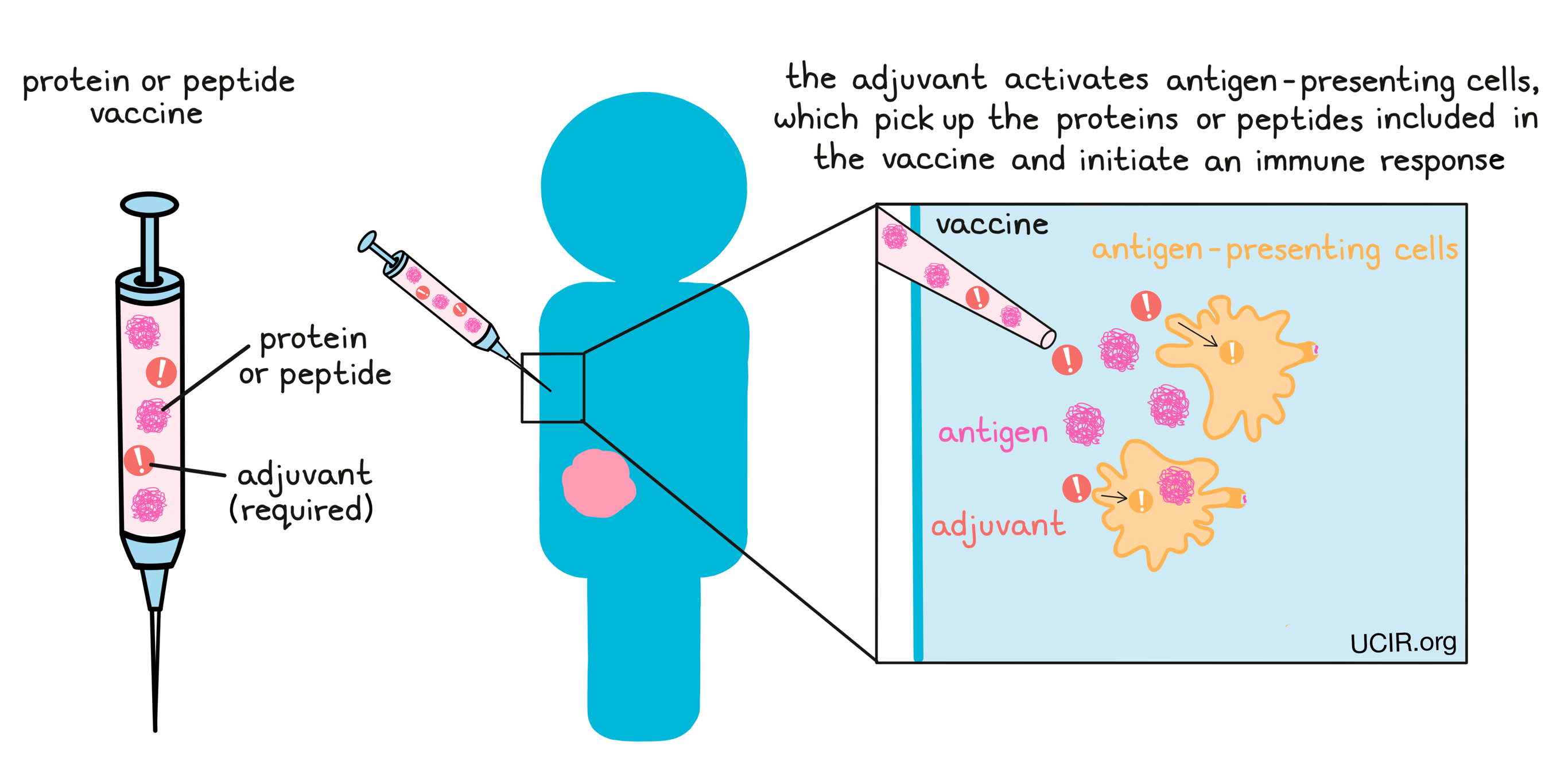
Once the antigens for a vaccine have been identified and chosen, they need to be incorporated into the vaccine itself. Antigens are protein molecules made up of individual building blocks – one of 20 different amino acids – joined together in a particular order. Different parts of the immune system are able to recognize either whole proteins or fragments of proteins called peptides. Proteins and peptides can be incorporated into vaccines directly, by using the tumor as the source of the proteins or peptides, or indirectly, by producing synthetic proteins or peptides in a laboratory.
When protein- or peptide-based vaccines are delivered to a patient, the adjuvant activates antigen-presenting cells, which pick up the vaccine proteins or peptides and initiate an immune response against the antigens.
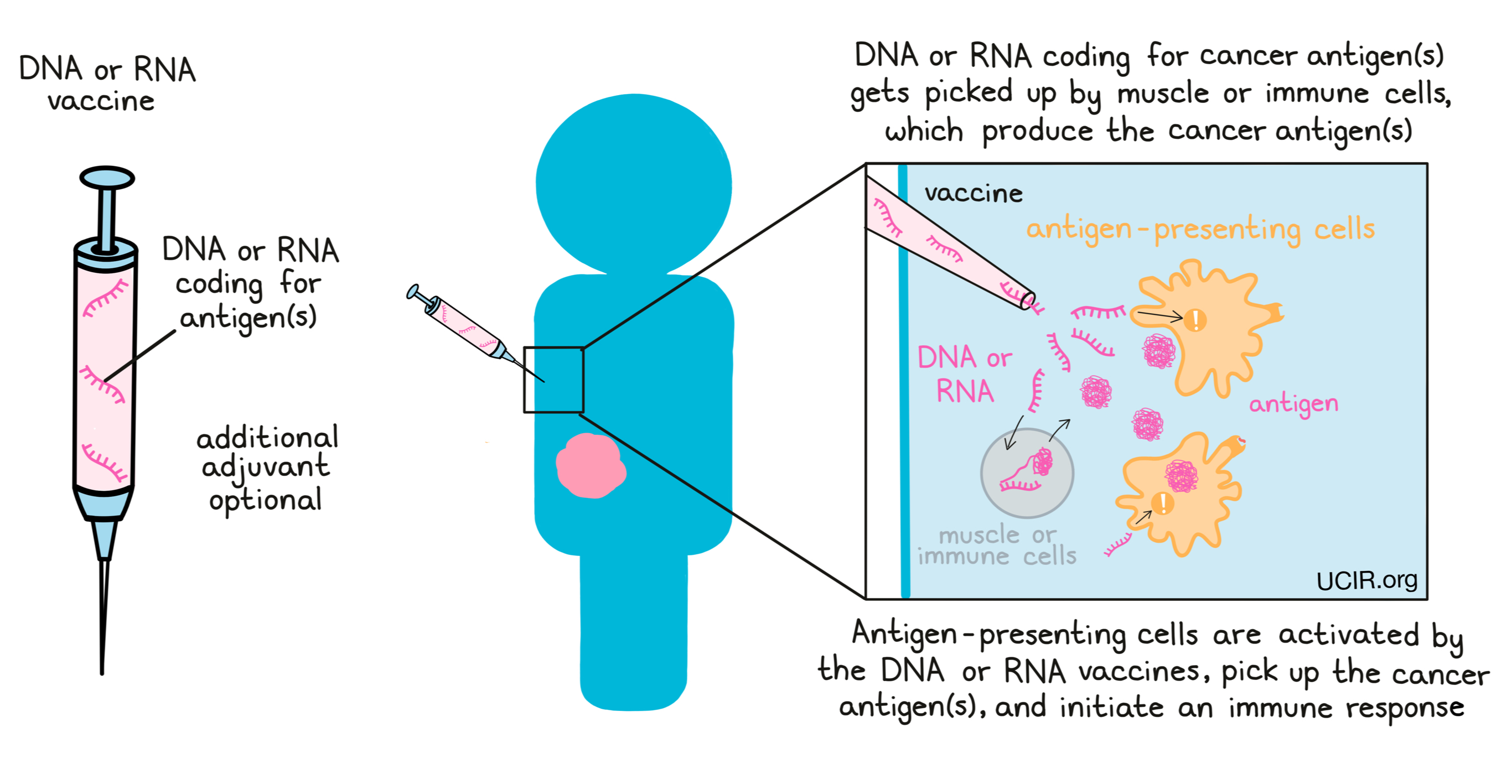
Alternatively, some vaccines are made using DNA or RNA, which code for the cancer antigens. In these cases, the DNA or RNA vaccine gets injected into the patient and picked up by muscle cells at the injection site or by immune cells. These cells then “read” the code, and begin to produce the cancer antigens. Then, as with protein or peptide vaccines, antigen-presenting cells pick up the antigens and initiate an immune response against them. This strategy offers several advantages in the production of vaccines, as making DNA and RNA in a laboratory is generally easier, faster, and cheaper than making whole proteins or peptides. Further, DNA and RNA can act as adjuvants themselves, so the inclusion of an additional adjuvant is optional.
Delivering the vaccine
A key objective in cancer vaccination is to deliver the cancer antigens in a way that catches the attention of the immune system. It is particularly important for a vaccine to activate antigen-presenting cells, which can engulf the antigens from the vaccine and carry them to the lymph nodes, initiating the strong B cell and T cell attacks that can target and destroy cancer cells. In efforts to elicit strong immune responses, researchers have developed a number of strategies for vaccine delivery. Depending on the type of the delivery system, vaccines can be injected under the skin, into the muscle, into the tumor, into the lymph node, or into the bloodstream.
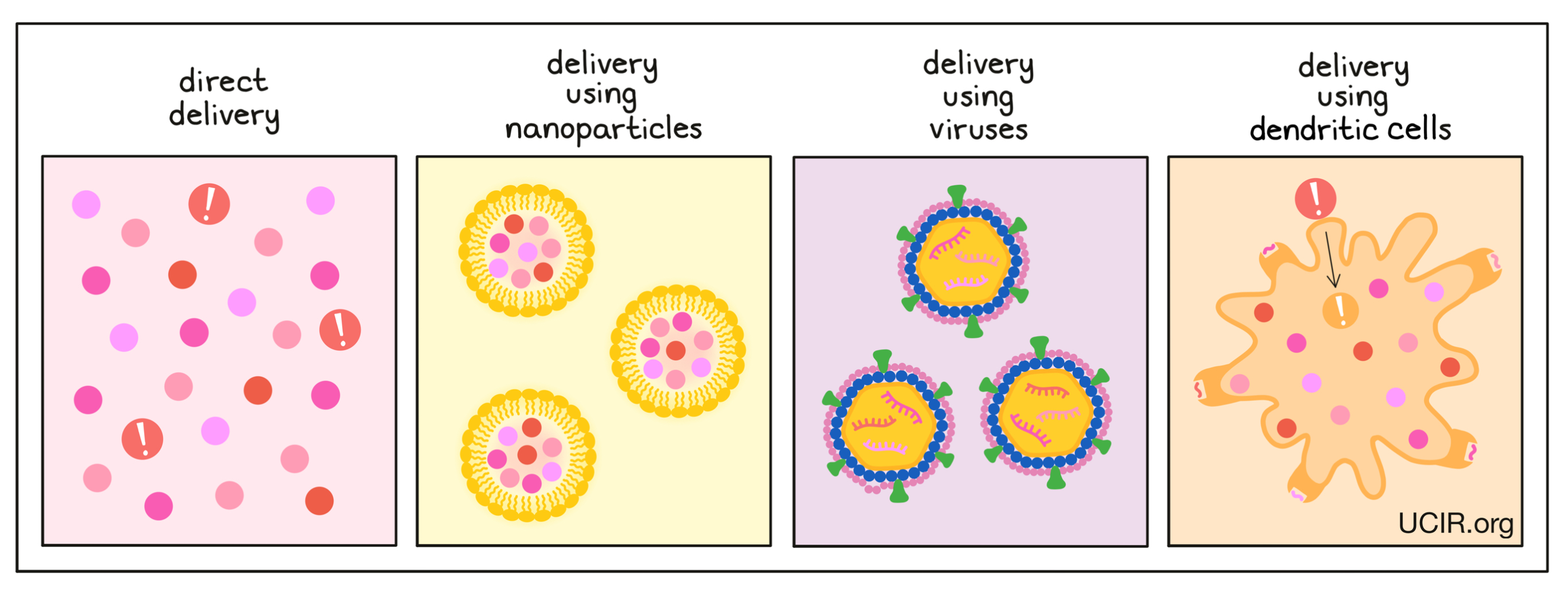
Direct delivery:
The most direct and most commonly used vaccine delivery approach is to mix protein or peptide antigens with an adjuvant and inject it into the patient, where antigen-presenting cells, like dendritic cells, pick up the antigens, become activated by the adjuvant, and initiate an immune response. Direct delivery can also be used for DNA and RNA vaccines.
Delivery using nanoparticles:
Antigens and adjuvants can also be packaged into nanoparticles – tiny bubbles made of fatty material that is naturally present in the body. Nanoparticles can help to protect antigens from premature degradation in the body, and can act as the vaccine adjuvant, catching the attention of nearby immune cells.
Delivery using viruses:
Antigens may also be incorporated into weakened viruses or shells of viruses. In these cases, the DNA or RNA encoding the cancer antigens is incorporated into the DNA or RNA of the virus. Since viruses naturally attack and enter cells, this can be an efficient way to deliver antigen-encoding DNA or RNA into cells. Additionally, viruses carry their own antigens, which are easily recognized by the immune system. They also generate danger signals, acting as an adjuvant for the vaccine.
Delivery using dendritic cells:
Some types of antigen-presenting cells, such as dendritic cells, can be isolated from a patient's blood and grown in a laboratory, where researchers can feed the dendritic cells the antigens of their choice, as well as treat them with adjuvants to activate them and enhance their ability to initiate strong immune responses. The dendritic cells themselves can then be injected back into the patient, where they go on to activate strong immune responses to the cancer antigens they now carry.
Cancer vaccines in the clinic
Sipuleucel T (Provenge) is a cancer vaccine used to treat men with advanced prostate cancer. It is the only therapeutic cancer vaccine currently approved by the FDA.
Many clinical trials have tested different types of cancer vaccines. In some patients, a clinical benefit was observed, along with evidence that their immune system had been activated against their cancer. However, so far there has been limited success in curing patients. The majority of these trials have been conducted with cancer-associated antigens. As described above, cancer-associated antigens are “self”-antigens and, hence, do not induce strong immune responses.
More recent studies showing clinical responses to neoantigen vaccines have created significant excitement, and it is hoped that new and improved methods for identifying more and stronger neoantigens will improve cancer vaccines and further enhance responses to therapy. However, larger studies with longer follow-up times will be required to be confident that the encouraging early clinical results will result in patient benefits.
New directions for cancer vaccines
Vaccines using neoantigens, which the immune system sees as foreign, have shown early encouraging results and are currently a major research focus. These vaccines have been “personalized”, meaning that because the mutations in each patient are almost entirely different from the mutations in another patient, a new vaccine has to be prepared for each patient. Neoantigens are identified by comparing the code of the DNA of each patient’s tumor with the code of the DNA of each patient’s healthy tissue to identify mutations and then using tests to decide which antigens will be included in the vaccine. Sometimes those tests even use the patient’s own immune cells in a laboratory setting to select antigens that can cause a significant immune response. This process is time-intensive (months) and expensive, and strategies to streamline the process are needed.
Recent encouraging results have also been seen with some versions of whole cancer cell vaccines, which naturally contain all the neoantigens and cancer-associated antigens of the cancer. However, the logistics, time, and cost of preparing these vaccines is also a challenge to overcome.
There are a small number of neoantigens that are shared among many patients. These are due to mutations in genes that are involved in helping the cancer cells multiply and survive. Identifying such shared neoantigens is an important ongoing quest.
For each of these described vaccine approaches, the dose of the vaccine and whether and how often additional “booster” vaccinations are given, can further optimize the strength of immune responses. Additional strategies to consider and test include how and when to combine cancer vaccine use with existing therapies, as well as with other promising cancer immunotherapies.
Finally, the development of vaccines that can prevent cancer, or at least some types of cancer, is an important research goal.
There is one existing vaccine that does prevent cancer. The human papillomavirus (HPV) can cause several forms of cancer. A vaccine against HPV can prevent most cases of cervical cancer and head and neck cancer, and is widely used to vaccinate women and men throughout the world. However, the vast majority of cancers are not caused by a virus.
Further information
UCIR news story:
- Can a cancer vaccine keep ovarian cancer at bay?
- Two approaches share one common target: efforts to fight childhood glioma
- mRNA vaccines: from cancer immunotherapy to COVID-19
Videos/websites:
- Cancer Vaccines; Memorial Sloan Kettering Cancer Center (video)
- Preventative vaccines in general and HPV & its Vaccine; Memorial Sloan Kettering Cancer Center (video)
- Cancer Treatment Vaccines, National Cancer Institute
Scientific references:
- Identifying and Targeting Human Tumor Antigens for T Cell-Based Immunotherapy of Solid Tumors (review article)
- Personal neoantigen cancer vaccines: a road not fully paved (review article)
- Therapeutic cancer vaccines (review article)
- Cancer vaccines: Building a bridge over troubled waters (review article)


